LYME, LEPRA Y SIFILIS, LOS ESLABONES PERDIDOS. !!
LYME, LEPROSY AND SYPHILIS, THE MISSING LINKS. !!
EDITORIAL ESPAÑOL:
==================
Hola amigos de la red hoy el DERMAGIC EXPRESS te trae un tema bien caliente: ENFERMEDAD DE LYME, LEPRA Y SIFILIS, LOS ESLABONES PERDIDOS. Se trata de Tres (3) enfermedades ancestrales, apocalípticas, que probablemente existen desde la época bíblica y que tienen entre sí, elementos compartidos, los cuales te voy a explicar aquí.
ENFERMEDAD DE HANSEN O LEPRA:
===============================
La LEPRA, enfermedad ancestral y apocalíptica descrita en la SAGRADA BIBLIA, capitulo del LEVITICO 13:12 que reza así:
"...Y si la lepra brota y se extiende en la piel, y la lepra cubre toda la piel del que tenía la infección, desde su cabeza hasta sus pies, hasta donde pueda ver el sacerdote..."
Han pasado más de 2.000 años y todavía hay LEPRA en el mundo, siendo los países mas afectados LA INDIA, en el continente ASIATICO, y BRASIL en el continente AMERICANO.
En el año 1.783 el científico ARMAUER HANSEN describió el agente causal de esta enfermedad: EL BACILO MYCOBACTERIUM LEPRAE, enfermedad altamente contagiosa que obligo a los gobiernos de aquella época a AISLAR a estos pacientes en todo el mundo en sitios denominados LEPROSERIAS. Es de notar que este agente causal NUNCA HA PODIDO SER CULTIVADO a diferencia de otros... En el año 2.008 se descubrió otra cepa el MYCOBACTERIUM LEPROMATOSIS, también agente causal de esta enfermedad.
El primer tratamiento que se utilizo fue el ACEITE DE CHALMOOGRA introducido por el Egipcio Tortoulis Bey in 1.894. Se intentaron otros tratamientos hasta que miles de años después en los años 70 fueron cerrados cuando fueron descubiertas TRES grandes medicinas que HOY DIA todavía se utilizan en el tratamiento:
1.) LA DAPSONA o DIAMINODIFENIL SULFONA (DDS), con el nombre comercial de PROMIN, componente químico GLUCOSULFONA DE SODIO (laboratorio Parke Davis) nombre comercial PROMIN, en el año 1.940, cuando todavía no existía tratamiento efectivo para esta enfermedad.
2. Y 3.) En los años 1.950 aparecen los medicamentos CLOFAZIMINA (1.953) con el nombre comercial LAMPRENE y RIFAMPICINA 1.957), altamente efectivos contra EL MYCOBACTERIUM LEPRAE y se instaura el llamado tratamiento MTD (MULTI DRUGS THERAPY) con estas tres medicinas, con un buen margen de éxito contra esta estigmatizante y bíblica enfermedad, el cual TODAVIA es utilizado hoy en día, en combinación con otros entre ellos LA MINOCICLINA, CLARITROMIINA, OFLOXACINA Y AMOXICILINA.
El CLOFAZIMINE fue aprobado por la FDA para sus uso en Estados Unidos en 1.986, y la RIFAMPICINA en 1.971
El descubrimiento de estas TRES (3) MEDICINAS: DAPSONA+CLOFAZIMINA+ RIFAMPICINA decreto el cierre de las LEPROSERIAS EN TODO EL MUNDO. Leer acá los otros interesantes LINKS SOBRE LEPRA:
1.) LEPRA EN LA ISLA DE PROVIDENCIA.
2.) LEPRA EN CABO BLANCO.
3.) LEPRA 2.00 AÑOS DESPUES.
LA PALABRA LEPRA PROVIENE DE LA BIBLIA.
==================
Hola amigos de la red hoy el DERMAGIC EXPRESS te trae un tema bien caliente: ENFERMEDAD DE LYME, LEPRA Y SIFILIS, LOS ESLABONES PERDIDOS. Se trata de Tres (3) enfermedades ancestrales, apocalípticas, que probablemente existen desde la época bíblica y que tienen entre sí, elementos compartidos, los cuales te voy a explicar aquí.
ENFERMEDAD DE HANSEN O LEPRA:
===============================
La LEPRA, enfermedad ancestral y apocalíptica descrita en la SAGRADA BIBLIA, capitulo del LEVITICO 13:12 que reza así:
"...Y si la lepra brota y se extiende en la piel, y la lepra cubre toda la piel del que tenía la infección, desde su cabeza hasta sus pies, hasta donde pueda ver el sacerdote..."
Han pasado más de 2.000 años y todavía hay LEPRA en el mundo, siendo los países mas afectados LA INDIA, en el continente ASIATICO, y BRASIL en el continente AMERICANO.
En el año 1.783 el científico ARMAUER HANSEN describió el agente causal de esta enfermedad: EL BACILO MYCOBACTERIUM LEPRAE, enfermedad altamente contagiosa que obligo a los gobiernos de aquella época a AISLAR a estos pacientes en todo el mundo en sitios denominados LEPROSERIAS. Es de notar que este agente causal NUNCA HA PODIDO SER CULTIVADO a diferencia de otros... En el año 2.008 se descubrió otra cepa el MYCOBACTERIUM LEPROMATOSIS, también agente causal de esta enfermedad.
El primer tratamiento que se utilizo fue el ACEITE DE CHALMOOGRA introducido por el Egipcio Tortoulis Bey in 1.894. Se intentaron otros tratamientos hasta que miles de años después en los años 70 fueron cerrados cuando fueron descubiertas TRES grandes medicinas que HOY DIA todavía se utilizan en el tratamiento:
1.) LA DAPSONA o DIAMINODIFENIL SULFONA (DDS), con el nombre comercial de PROMIN, componente químico GLUCOSULFONA DE SODIO (laboratorio Parke Davis) nombre comercial PROMIN, en el año 1.940, cuando todavía no existía tratamiento efectivo para esta enfermedad.
2. Y 3.) En los años 1.950 aparecen los medicamentos CLOFAZIMINA (1.953) con el nombre comercial LAMPRENE y RIFAMPICINA 1.957), altamente efectivos contra EL MYCOBACTERIUM LEPRAE y se instaura el llamado tratamiento MTD (MULTI DRUGS THERAPY) con estas tres medicinas, con un buen margen de éxito contra esta estigmatizante y bíblica enfermedad, el cual TODAVIA es utilizado hoy en día, en combinación con otros entre ellos LA MINOCICLINA, CLARITROMIINA, OFLOXACINA Y AMOXICILINA.
El CLOFAZIMINE fue aprobado por la FDA para sus uso en Estados Unidos en 1.986, y la RIFAMPICINA en 1.971
El descubrimiento de estas TRES (3) MEDICINAS: DAPSONA+CLOFAZIMINA+ RIFAMPICINA decreto el cierre de las LEPROSERIAS EN TODO EL MUNDO. Leer acá los otros interesantes LINKS SOBRE LEPRA:
1.) LEPRA EN LA ISLA DE PROVIDENCIA.
2.) LEPRA EN CABO BLANCO.
3.) LEPRA 2.00 AÑOS DESPUES.
LA PALABRA LEPRA PROVIENE DE LA BIBLIA.
ENFERMEDAD DE LYME:
====================
Si tú piensas que la enfermedad de LYME fue descubierta en 1.981 cuando Willy Burgdorfer describió el agente causal de esta enfermedad, la ESPIROQUETA BORRELIA, que lleva como apellido su nombre BURGDORFERI en honor al descubridor, estas equivocado.
Las GARRAPATAS como peste también están descritas en la SAGRADA BIBLIA, en EL LIBRO DE EXODO, se hace referencia a las plagas que enviaría dios al Faraón de Egipto, entre ellas están ranas, tábanos, langostas, piojos y mosquitos...."
"...y el polvo de la tierra se convirtió en piojos por todo el país de Egipto"... un turista bien conocedor de Egipto observó que la arena parecía moverse; observando más detenidamente, vio que la superficie de la tierra era una masa de diminutas garrapatas..."
Las primeras descripciones de la ENFERMEDAD DE LYME datan de le época post-colonial en Nueva Inglaterra: región geográfica que comprende seis estados del noreste de los Estados Unidos: Maine, Vermont, New Hampshire, Massachusetts, Rhode Island y Connecticut, y de allí se disemino posteriormente al medio oeste.
Las primeras descripciones datan de los años 1.663 hasta 1.670, en Nueva Inglaterra, por John Josselyn, posteriormente en 1.749, Peter Kalm botánico Sueco en los bosques de Nueva York. 100 años después, los bosques habían desaparecido y la bacteria de Lyme probablemente se había aislado en algunos focos a lo largo de la costa noreste, Wisconsin y Minnesota.
Pero La primera Descripción de LA ENFERMEDAD DE LYME más exacta, data del año 1.764 por el Reverendo John Walker en la Isla de Jura (Isla de los Ciervos) en Escocia. Muchas personas de esta área de Gran Bretaña emigraron a América del Norte a partir del año 1717.
Se encontró ADN de BORRELIA en una GARRAPATA IXODES RICINUS en Alemania que data del año 1.884, en un ratón infectado que murió en 1.894, y mas allá de esto en la autopsia de la Momia Ötzi "Hombre de Hielo" (5.300 años) en el año 2.010 se encontró secuencias de ADN de BORRELIA BURGDORFERI, prueba fehaciente de que se trata de una plaga BIBLICA, convirtiéndose esta momia en el humano más antiguo con ENFERMEDAD DE LYME.
La palabra LYME proviene de un pueblo de Connecticut que lleva ese nombre donde aparecieron los primeros casos descritos como ARTRITIS DE LYME, o ERITEMA MIGRANS
====================
Si tú piensas que la enfermedad de LYME fue descubierta en 1.981 cuando Willy Burgdorfer describió el agente causal de esta enfermedad, la ESPIROQUETA BORRELIA, que lleva como apellido su nombre BURGDORFERI en honor al descubridor, estas equivocado.
Las GARRAPATAS como peste también están descritas en la SAGRADA BIBLIA, en EL LIBRO DE EXODO, se hace referencia a las plagas que enviaría dios al Faraón de Egipto, entre ellas están ranas, tábanos, langostas, piojos y mosquitos...."
"...y el polvo de la tierra se convirtió en piojos por todo el país de Egipto"... un turista bien conocedor de Egipto observó que la arena parecía moverse; observando más detenidamente, vio que la superficie de la tierra era una masa de diminutas garrapatas..."
Las primeras descripciones de la ENFERMEDAD DE LYME datan de le época post-colonial en Nueva Inglaterra: región geográfica que comprende seis estados del noreste de los Estados Unidos: Maine, Vermont, New Hampshire, Massachusetts, Rhode Island y Connecticut, y de allí se disemino posteriormente al medio oeste.
Las primeras descripciones datan de los años 1.663 hasta 1.670, en Nueva Inglaterra, por John Josselyn, posteriormente en 1.749, Peter Kalm botánico Sueco en los bosques de Nueva York. 100 años después, los bosques habían desaparecido y la bacteria de Lyme probablemente se había aislado en algunos focos a lo largo de la costa noreste, Wisconsin y Minnesota.
Pero La primera Descripción de LA ENFERMEDAD DE LYME más exacta, data del año 1.764 por el Reverendo John Walker en la Isla de Jura (Isla de los Ciervos) en Escocia. Muchas personas de esta área de Gran Bretaña emigraron a América del Norte a partir del año 1717.
Se encontró ADN de BORRELIA en una GARRAPATA IXODES RICINUS en Alemania que data del año 1.884, en un ratón infectado que murió en 1.894, y mas allá de esto en la autopsia de la Momia Ötzi "Hombre de Hielo" (5.300 años) en el año 2.010 se encontró secuencias de ADN de BORRELIA BURGDORFERI, prueba fehaciente de que se trata de una plaga BIBLICA, convirtiéndose esta momia en el humano más antiguo con ENFERMEDAD DE LYME.
La palabra LYME proviene de un pueblo de Connecticut que lleva ese nombre donde aparecieron los primeros casos descritos como ARTRITIS DE LYME, o ERITEMA MIGRANS
SIFILIS ETAPA PRIMARIA (CHANCRO) Y SECUNDARIA LESIONES EN COLLARETE EN PALMAS Y PLANTAS, Y ALOPECIA APOLILLADA
LA SIFILIS:
========
La enfermedades de transmisión sexual SIFILIS Y GONORREA, también están mencionadas en la BIBLIA, en el libro de GENESIS: 12, donde hace referencia a SARA, esposa de ABRAHAM contagiada con una enfermedad de transmisión sexual, que posteriormente se extendió a la corte del Faraón y sus concubinas; también en el LEVITICO, antiguo testamento capitulo 15 dice lo siguiente"
"....Moisés y Aarón recibieron de Yahvé sobre este punto: «hablad a los hijos de Israel y decidles: cualquier hombre que padezca flujo seminal en su carne será inmundo. Esta es la ley de su inmundicia en el flujo, ya sea porque su carne destile el flujo, ya por retenerlo. Es inmundo…" probablemente se referían a estas dos enfermedades, las cuales posteriormente fueron descritas como entidades separadas.
El origen exacto de la SIFILIS está en disputa. Se dice que hay dos teorías, una precolombina, que la ubica en Europa antes del viaje de Cristóbal Colón a las Américas, y otra Colombina, asociada a su viaje a las Américas, donde fue llevada a Europa por los tripulantes contagiados.
En 1.530 fue que el término "SIFILIS" fue utilizado por primera vez por el médico y poeta italiano Girolamo Fracastoro, y HACE REFERENCIA al personaje de una obra, llamada: "Sífilis o la enfermedad francesa" quien hace referencia a un personaje llamado SYPHILO, castigado por los dioses a sufrir una terrible enfermedad. El poema trata de los estragos de la enfermedad en ITALIA en esa época, específicamente en la ciudad de Nápoles en los años 1944 y 1945, durante la invasión Francesa.
El agente causal TREPONEMA PALLIDUM, es una ESPIROQUETA al igual que la ENFERMEDAD DE LYME y fue descubierto por Fritz Schaudinn y Erich Hoffmann en 1905. En 1.910 apareció el primer tratamiento para la SIFILIS denominado Salvarsán, (arsfenamina o compuesto 606) por el Alemán Paul Erlich, un derivado del arsénico, quien le hizo ganar el premio nobel de Medicina, y que se popularizo con el nombre de "BALA MAGICA".
Posteriormente se utilizaron las sales mercuriales a partir de 1.912, luego el Bismuto a partir de 1.922. La QUININA tratamiento para la malaria también fue utilizada en la sífilis terciaria o NEUROSIFILIS y este tratamiento le hizo ganar el premio nobel de medicina a Julius Wagner-Jauregg en 1.927.
EN 1.928 aparece la noble PENICILINA descubierta por ALEXANDER FLEMING, la cual comenzó a usarse en la SIFILIS en 1.943, siendo hoy día TODAVIA la primera elección de tratamiento para esta enfermedad.
Se dice que personajes famosos como: Franz Schubert, Al Capone y Édouard Manet tuvieron la enfermedad.
LA PALABRA SIFILIS proviene del LATIN: SIPH: CERDO. PHILUS: AMOR
LA SIFILIS Y ENFERMEDAD DE LYME:
================================
A.) Ambas enfermedades son producidas POR ESPIROQUETAS, en el caso de de la SIFILIS, EL TREPONEMA PALLIDUM PALLIDUM, en el caso de LYME LA BORRELIA BURGDORFERI.
B.) Ambas enfermedades se pueden transmitir en embarazadas al FETO.
C.) Ambas ESPIROQUETAS pueden ser detectadas por MICROSCOPIA OPTICA, "Campo oscuro" en la SIFILIS y "Color Azul" (Profesor Laane e Ivar Mysterud).
E.) No existen RESERVORIOS naturales para la SIFILIS, el principal HOSPEDADOR Y FUENTE DE CONTAGIO es el hombre y la transmisión es a través de RELACIONES SEXUALES y eventualmente TRANSFUSIONES SANGUINEAS de personas contaminadas. La fuente de CONTAGIO DE LA ENFERMEDAD DE LYME son GARRAPATAS y hay muchos animales que actúan como hospedadores entre ellos CIERVOS, AVES, y RATONES, también se han encontrado secuencias de ADN de BORRELIA en animales domésticos como PERROS, GATOS Y CABALLOS.
E.) Ambas ESPIROQUETAS se pueden detectar por exámenes de sangre:
- SIFILIS: VDRL, PCR, Inmunoensayo enzimático (IEA), FTA ABs.
- LYME: Western Blot (IgG, IgM, Multiplex PCR, ensayo inmunoabsorbente ligado a enzimas (ELISA), inmunoensayo enzimático (IEA), inmunofluorescencia indirecta IGg e IgM). IgA/IgG/IgM IFA Screen, Inmunoblot IgM, IgG, IGXspot, IgM, IgG 31 Kda Prueba de epitope.
E.) OTRA GRAN DIFERENCIA ENTRE AMBAS es que hoy día, después que la PENICILINA FUE DESCUBIERTA todavía sigue siendo la primera OPCION y el TREPONEMA PALLIDUM no ha generado REISTENCIA al antibiótico, también la DOXICICLINAy TETRACICLINAS son efectivas en la SIFILIS. Otro Detalle es que si bien el TREPONEMA presenta otras especies, solo el TREPONEMA PALLIDUM PALLIDUM es el agente causal de la SIFILIS.
C: En el caso de LA ENFERMEDAD DE LYME son muchas LAS ESPECIES DE BORRELIA que se han descrito en las diferentes aéreas geográficas del mundo las que ocasionan esta enfermedad, habiéndose descrito más de 52 especies en total. De las cuales 21 especies ya están reconocidas y distribuidas en todo el mundo:
De estas: 10 especies son patógenas para el humano, ellas son: B. afzelii, B. bavariensis, B. bissettii, B. burgdorferi sensu stricto, B. garinii, B. kurtenbachii, B. lusitaniae, B. mayonii, B. spielmanii, B. valaisiana, sin dejar de mencionar la Borrelia Miyamitoi causante de la FIEBRE RECURRENTE descrita en el año 1.994 y que en 2.011 se describió en Humanos en Rusia; Estados Unidos, Japón y Europa.
De estas, hay once (11) especies identificadas que aún no han sido detectadas o aisladas de humanos. Este grupo incluye B. americana, B. andersonii, B. californiensis, B. carolinensis, B. chilensis, B. finlandensis, B. japonica, B. tanukii, B. turdi, B. sinica y B. yangtze.
H.) LYME y SIFILIS comparten 3 etapas clinicas: PRIMARIA, SECUNDARIA y TARDIA (NEUROBORRELIOSIS Y NEUROSIFILIS)
LEPRA Y ENFERMEDAD DE LYME:
============================
A.) Ambas enfermedades o plagas son mencionadas en la BIBLIA.
B.) La LEPRA no se transmite de embarazadas al Feto; en la ENFERMEDAD DE LYME se ha descrito esta transmisión.
C.) Al igual que la SIFILIS, para la LEPRA existe un solo agente causal descrito por Armauer Hansen el MYCOBACTERIUM LEPRAE en 1.783 y 225 años después, año 2.008 se describe una sub-especie que se denomino MYCOBATERIUM LEPROMATOSIS. A Diferencia de la enfermedad de LYME que como ya describí su agente causal BORRELIA BURGORFERI, tiene muchas especies que afectan al humano.
D.) La LEPRA es altamente contagiosa de HUMANO A HUMANO, principalmente a través de secreción nasal, principal mecanismo de diseminación, y como reservorios naturales se describen el Armadillo de 9 bandas (Dasypus novemcinctus, Mycobacterium Leprae) y las Ardillas Rojas en las Islas Británicas (Mycobacterium Lepromatosis), pero repito esta enfermedad ancestral tiene al HOMBRE como su principal HOSPEDADOR y fuente de CONTAGIO.
Sin embargo en el Sudeste de los Estados Unidos en el año 2.015 se describieron varios casos de contagio del Armadillo de nueve (9) bandas a humanos de modo que tambien es considerada como una enfermedad zoonotica.
La enfermedad de LYME no se transmite de HUMANO-HUMANO, el VECTOR principal son GARRAPATAS en su mayoría y RESERVORIOS, animales ya descritos. Una de las grandes diferencias entre estas dos (2) plagas.
E.) El diagnostico de LA LEPRA se hace:
- CLINICAMENTE: tipo de lesiones.
- Examen de LINFA: Coloración de Giemsa.
- Biopsia de Piel: Coloración Hematoxilina Eosina (HE) y Faraco- Fite.
- Distribución Geográfica: aéreas Endémicas.
- Exámenes de Laboratorio: PCR.
Como dije anteriormente el diagnostico de la enfermedad de LYME aparte de las manifestaciones clínicas, se hace en base a pruebas de laboratorio MUCHAS DE LAS CUALES resultan en "NEGATIVO" siendo positivos los pacientes, Pues en las BIOPSIAS de las lesiones de piel en las que se sospecha y se ha confirmado por laboratorio el diagnostico NO SE DETECTA la BORRELIA en la mayoría de los casos a excepción del LINFOCITOMA por BORRELIA donde en biopsia de piel si se ha encontrado este agente causal. En las Biopsias de piel de los NODULOS LEPROSOS, en el 100% encuentras el Mycobaterium Leprae.
E.) EL MYCOBACTERIUM LEPRAE nunca ha podido ser cultivado. La BORRELIA BURGDROFERI si.
F.) La LEPRA tremenda plaga ha sido dominada y disminuido NOTABLEMENTE los casos en el mundo con el esquema MULTI-DROGAS: DAPSONA (SULFA), + CLOFAZIMINA + RIFAMIPICINA, en combinación con otros que ya mencione: OFLOXACINA, MINOCICLINA, CLARITROMICINA, y AMOXICILINA. Se han descrito casos de LEPRA resistentes al tratamiento clásico de (MTD) y Otros antimicrobianos. Con la ENFERMEDAD DE LYME ocurre exactamente lo mismo pero en mayor grado, debido probablemente a las numerosas especies de LA BORRELIA causantes de la enfermedad.
En la enfermedad de LYME se ha utilizado muy poco los esquemas de tratamiento ya mencionados en la enfermedad de HANSEN o la LEPRA.
LOS ESLABONES PERDIDOS:
========================
1.) CONFIRMACION DEL DIAGNOSTICO:
================================
Como te podrás dar cuenta esta es una de las GRANDES DIFERENCIAS ente SIFILIS, LEPRA Y LYME: EL DIAGNOSTICO SEROLOGICO, en la SIFILIS, es PRECISO Y EXACTO en la ENFERMEDAD DE LYME el CDC solo aprueba 2 tipos de test y muchos de ellos resultan en "NEGATIVO", y muchas veces después de otros exámenes es que el paciente resulta "POSITIVO" quizá cuando la enfermedad ya ha dañado tu organismo. En el caso de la LEPRA también el diagnostico de la enfermedad es en más de un 90% yo diría en su totalidad, también es PRECISO Y EXACTO Este es uno de los grandes problemas que está causando a nivel de salud pública esta en enfermedad: LA CONFIRMACION DEL DIAGNOSTICO.
2.) EFECTIVIDAD DEL TRATAMIENTO:
===============================
Como dije anteriormente LA SIFILIS hoy día, luego de 74 años de ser utilizada LA PENICILINA, para tratar esta enfermedad sigue siendo la PRIMERA OPCION , seguida de otros como doxiciclina y tetraciclinas. Quiere decir esto que el TREPONEMA PALLIDUM no ha desarrollado resistencia a este NOBLE ANTIBIOTICO.
En el caso de la Lepra la TRIPLE COMBINACION de DAPSONA+ CLOFAZIMINA+ RIFAMPICINA, durante años fue el puntal del tratamiento de la enfermedad hasta el punto que este hecho fue el que decreto (ya lo he dicho varias veces) el cierre de las LEPROSERIAS en el mundo. Posteriormente apareció la resistencia a estas medicinas, pero aparecieron otras como LA MINOCICLINA OFLOXACINA y otras para ayudar en el tratamiento.
Por el contrario en el caso de la ENFERMEDAD DE LYME, la BORRELIA, y sus múltiples especies es bien conocido como han desarrollado RESISTENCIA a muchos antibióticos, incluyendo DOXICICLINA, TETRACICLINAS, AMOXICILIA, PENICILINA y otros considerados altamente efectivos contra ella, siendo este hecho uno de los GRANDES DESAFIOS hoy día contra esta plaga hoy día.
3.) RESISTENCIA AL TRATAMIENTO:
=============================
1.) En la SIFILIS, prácticamente no existe resistencia a la PENICILINA BENZATINICA G. y otros utilizados, pues el TREPONEMA PALLIDUM PALLIDUM, no ha ofrecido mutaciones. Sigue siendo el mismo.
2.) En la LEPRA, ocurre casi igual que la SIFILIS, el Mycobacterium Leprae no ha Mutado, y pasaron 225 años para que se describiera la sub-especie: Mycobaterium Lepromatosis. Por lo tanto el CLASICO TRATAMIENTO Multy drug Therapy sigue siendo vigente (DAPSONA+CLOFAZIMINA+ RIFAMPICINA) con variaciones en los casos de resistencia que se describieron años después, donde se incluye en primer lugar la MINOCICLINA.
3.) En El caso de la enfermedad de LYME, el cuento es otro LA BORRELIA BURDORGFERI y sus especies han desarrollado RESISTENCIA a casi todos LOS tratamientos existentes, que ya he descrito en mis publicaciones previas. LOS CODIGOS DE LA ENFERMEDAD DE LYME. I Y II
CONCLUSIONES:
==============
Quizá te estés preguntando porque hice esta triple comparación: LYME, LEPRA, Y SIFILIS, y como siempre te voy a dar la respuesta.
1.) Son enfermedades reseñadas en la BIBLIA como "PLAGAS" o males enviados por Dios al ser humano, enfermedades ancestrales y APOCALIPTICAS.
2.) Aun habiéndose logrado descubrir sus agentes causales y tratamientos: estas plagas LYME SIFILIS Y LEPRA, siguen existiendo en el mundo entero.
3.) La SIFILIS Y LEPRA muestran todavía una alta sensibilidad a los tratamientos CONOCIDOS
4.) LYME, es la que presenta mayor dificultad en diagnostico SEROLOGICO y TRATAMIENTO por el desarrollo de resistencia y la "habilidad" de esta Espiroqueta de "evadir" las pruebas diagnosticas.
5.) En la presente revisión veo que la DAPSONA (DIAMINODIFENILSULFONA (DDS) droga que prácticamente ha abatido a la LEPRA no está siendo UTILIZADA frecuentemente en la enfermedad de LYME, han desestimado su uso, habiéndose descrito la SENSIBILIDAD DE LA BORRELIA a esta droga. Fin de la historia:
DAPSONA+ CLOFAZIMINA+ RiFAMPICINA, o DAPSONA+ MINOCICLINA+ CLOFAZIMINA deben ser utilizadas en la enfermedad de LYME.
"... todo lo que a la tierra le quitareis, la tierra te lo devolverá, si no ayudas a tu vecino, abatido por cualquier plaga, pronto las plagas se volverán en contra tuya, tu vecino será libre y tu vivirás las cadenas que aquellos vi vivieron..."
palabras BIBLICAS.
Saludos a todos.
Dr. José Lapenta.
Saludos a todos.
Dr. José Lapenta.
Dr. José M. Lapenta.
ENGLISH EDITORIAL:
=================
Hello friends of the network today DERMAGIC EXPRESS brings you a hot topic: LYME DISEASE, LEPROSY AND SYPHILIS, THE MISSING LINKS. It is about three (3) ancestral, apocalyptic diseases, which probably exist since the biblical era and have shared elements among them, which I will explain here.
HANSEN DISEASE OR LEPROSY:
===========================
The LEPROSY, ancestral and apocalyptic disease described in HOLY BIBLE, chapter of LEVITICUS 13:12 that reads as follows:
"... And if the leprosy break out abroad in the skin, and the leprosy cover all the skin of him that hath the plague from his head even to his feet, as far as appeareth to the priest...
More than 2,000 years have passed and there is still LEPROSY in the world, with the most affected countries being INDIA, in the ASIAN continent, and BRAZIL in the AMERICAN continent.
In 1.783 the scientist ARMAUER HANSEN described the causative agent of this disease: THE MYCOBACTERIUM LEPRAE BACILLUS, a highly contagious disease that forced the governments of that time to isolate these patients all over the world in places called LEPROSERIES. It is noteworthy that this causal agent has NEVER COULD BE CULTIVATED unlike others. In the year 2.008, (225 years later) another strain was discovered MYCOBACTERIUM LEPROMATOSIS, also causal agent of this disease.
The first treatment that was used was the CHALMOOGRA OIL introduced by the Egyptian Tortoulis Bey in 1.894. Other treatments were tried until thousands of years, later in the 70s before THE LEPROSERIES were closed: they were discovered THREE great medicines that TODAY DAY are still used in the treatment:
1.) DAPSONE or DIAMINODIPHENYLSULFONE (DDS), with the commercial name of PROMIN, chemical component SODIUM GLUCOSULFONE (laboratory Parke Davis) commercial name PROMIN, in the year 1.940, when there was still no effective treatment for this disease.
2. and 3.) In the years 1.950s, the drugs CLOFAZIMINE (1.953) under de commercial name LAMPRENE and RIFAMPICIN (1.957) appeared, highly effective against MYCOBACTERIUM LEPRAE and the so-called treatment MTD (MULTI DRUGS THERAPY) was established with these three medicines, with a good margin of success against this stigmatizing and biblical disease, which STILL is used today, in combination with others including MINOCYCLINE, CLARYTHROMICIN, OFLOXACIN AND AMOXICILIN.
CLOFAZIMINE was approved by the FDA for use in the United States in 1.986 and RIFAMPICIN in 1.971
The discovery of these THREE (3) MEDICINES: DAPSONE + CLOFAZIMINE + RIFAMPICIN decreed the closure of LEPROSERIES WORLDWIDE. Read here the other interesting LINKS ABOUT LEPROSY:
1.) LEPROSY ON THE ISLAND OF PROVIDENCIA.
2.) LEPROSY IN CAPE WHITE.
3.) LEPROSY 2.00 YEARS LATER
THE WORD LEPROSY COMES FROM THE BIBLE.
=================
Hello friends of the network today DERMAGIC EXPRESS brings you a hot topic: LYME DISEASE, LEPROSY AND SYPHILIS, THE MISSING LINKS. It is about three (3) ancestral, apocalyptic diseases, which probably exist since the biblical era and have shared elements among them, which I will explain here.
HANSEN DISEASE OR LEPROSY:
===========================
The LEPROSY, ancestral and apocalyptic disease described in HOLY BIBLE, chapter of LEVITICUS 13:12 that reads as follows:
"... And if the leprosy break out abroad in the skin, and the leprosy cover all the skin of him that hath the plague from his head even to his feet, as far as appeareth to the priest...
More than 2,000 years have passed and there is still LEPROSY in the world, with the most affected countries being INDIA, in the ASIAN continent, and BRAZIL in the AMERICAN continent.
In 1.783 the scientist ARMAUER HANSEN described the causative agent of this disease: THE MYCOBACTERIUM LEPRAE BACILLUS, a highly contagious disease that forced the governments of that time to isolate these patients all over the world in places called LEPROSERIES. It is noteworthy that this causal agent has NEVER COULD BE CULTIVATED unlike others. In the year 2.008, (225 years later) another strain was discovered MYCOBACTERIUM LEPROMATOSIS, also causal agent of this disease.
The first treatment that was used was the CHALMOOGRA OIL introduced by the Egyptian Tortoulis Bey in 1.894. Other treatments were tried until thousands of years, later in the 70s before THE LEPROSERIES were closed: they were discovered THREE great medicines that TODAY DAY are still used in the treatment:
1.) DAPSONE or DIAMINODIPHENYLSULFONE (DDS), with the commercial name of PROMIN, chemical component SODIUM GLUCOSULFONE (laboratory Parke Davis) commercial name PROMIN, in the year 1.940, when there was still no effective treatment for this disease.
2. and 3.) In the years 1.950s, the drugs CLOFAZIMINE (1.953) under de commercial name LAMPRENE and RIFAMPICIN (1.957) appeared, highly effective against MYCOBACTERIUM LEPRAE and the so-called treatment MTD (MULTI DRUGS THERAPY) was established with these three medicines, with a good margin of success against this stigmatizing and biblical disease, which STILL is used today, in combination with others including MINOCYCLINE, CLARYTHROMICIN, OFLOXACIN AND AMOXICILIN.
CLOFAZIMINE was approved by the FDA for use in the United States in 1.986 and RIFAMPICIN in 1.971
The discovery of these THREE (3) MEDICINES: DAPSONE + CLOFAZIMINE + RIFAMPICIN decreed the closure of LEPROSERIES WORLDWIDE. Read here the other interesting LINKS ABOUT LEPROSY:
1.) LEPROSY ON THE ISLAND OF PROVIDENCIA.
2.) LEPROSY IN CAPE WHITE.
3.) LEPROSY 2.00 YEARS LATER
THE WORD LEPROSY COMES FROM THE BIBLE.
LYME'S DISEASE:
===============
If you think that the LYME disease was discovered in 1.981 when Wllly Burgdorfer described the causative agent of this disease, the ESPIROCHETE BORRELIA, whose name is BURGDORFERI in honor of the discoverer, you are wrong.
The TICKS as a plague are also described in the HOLY BIBLE, in THE BOOK OF EXODUS, reference is made to the plagues that God would send to the Pharaoh of Egypt, and among them are frogs, horsefly, lobsters, lice and mosquitoes .... "
"... And the dust of the earth became lice throughout the land of Egypt" ... a well-knowledgeable tourist from Egypt observed that the sand seemed to move; observing more closely, he saw that the surface of the earth was a mass of tiny ticks ... "
The first descriptions of LYME DISEASE date from the post-colonial era in New England: geographic region comprising six states of the Northeast of the United States: Maine, Vermont, New Hampshire, Massachusetts, Rhode Island and Connecticut, and from there I later disseminated to the Midwest.
The first descriptions date from the years 1,663 to 1,670, in New England, by John Josselyn, later in 1.749, Peter Kalm Swedish botanist in the forests of New York. 100 years later, the forests had disappeared and the Lyme bacteria had probably been isolated in some outbreaks along the northeast coast, Wisconsin and Minnesota.
But the first description of the most accurate LYME DISEASE dates from the year 1.764 by the Reverend John Walker on the Isle of Jura (Island of the Deer) in Scotland. Many people from this area of Great Britain emigrated to North America from the year 1.717.
BORRELIA DNA was found in an IXODES RICINUS TICKS in Germany dating from the year 1.884, in an infected mouse that died in 1.894, and beyond this in the autopsy of the Ötzi Mummy "Ice Man" (5,300 years) in the year 2.010 was found DNA sequences of BORRELIA BURGDORFERI, proof that it is a BIBLICAL pest, this mummy become the oldest human with LYME DISEASE.
The word LYME comes from a town in Connecticut that bears that name where the first cases described as ARTHRITIS OF LYME appeared, or ERYTHEMA MIGRANS.
THE SYPHILIS:
============
Sexually transmitted diseases SYPHILIS AND GONORRHEA, are also mentioned in the BIBLE, in the book GENESIS: 12, which refers to SARA, wife of ABRAHAM infected with a sexually transmitted disease, which later spread to the court of Pharaoh and his concubines; also in the LEVITICUS, Old Testament chapter 15 says the following”
"... Moses and Aaron received from Yahweh on this point:" Speak to the children of Israel and say to them, "Any man who has a seminal discharge in his flesh will be unclean." This is the law of his uncleanness in the flow, either because his flesh distills the flow, or by holding it in. It is unclean ... "They were probably referring to these two diseases, which were later described as separate entities.
The exact origin of the SYPHILIS is in dispute. It is said that there are two theories, one pre-Columbian, that locates it in Europe before the trip of Christopher Columbus to the Americas, and another Columbine, associated with his trip to the Americas, where he was taken to Europe by the infected crew.
In 1.530 it was that the term "SYPHILIS" was used for the first time by the Italian doctor and poet Girolamo Fracastoro, and REFERS to the character of a work, called: " Syphilis or the French disease "who refers to a character called SYPHILUS , punished by the gods to suffer a terrible disease. The poem deals with the ravages of the disease in ITALY at that time, specifically in the city of Naples in the years 1,944 and 1.945, during the French invasion.
The causal agent TREPONEMA PALLIDUM is an ESPIROCHETE as well as LYME DISEASE and was discovered by Fritz Schaudinn and Erich Hoffmann in 1.905. In 1.910 the first treatment for SYPHILIS named Salvarsan, (arsphenamine or compound 606) by German Paul Erlich, a derivative of arsenic, who won him the Nobel Prize for Medicine, and which was popularized with the name "MAGIC BULLET".
Subsequently, the mercurial salts were used from 1.912, then Bismuth from 1.922. The QUININE treatment for malaria was also used in the tertiary syphilis or NEUROSYPHILIS and this treatment won him the Nobel Prize for medicine to Julius Wagner-Jauregg in 1.927.
IN 1.928 appears the noble PENICILLINE discovered by ALEXANDER FLEMING, which began to be used in the SYPHILIS in 1.943, being today STILL the first choice of treatment for this disease.
It is said that famous people like: Franz Schubert, Al Capone and Édouard Manet had the disease.
THE WORD SYPHILIS comes from LATIN: SIPH: PIG. PHILUS: LOVE
THE SYPHILIS AND LYME'S DISEASE:
==============================
A.) Both diseases are produced by ESPIROCHETES, in the case of the SYPHILIS, the TREPONEMA PALLIDUM PALLIDUM, in the case of LYME the BORRELIA BURGDORFERI.
B.) Both diseases can be transmitted in pregnant women to the FETUS.
C.) Both ESPIROHETES can be detected by OPTIC MICROSCOPY, "Dark Field" in SYPHILIS and "Blue Color staining" (Professor Laane and Ivar Mysterud).
D.) There are no natural HOSTS for the SYPHILIS, the main RESERVOIR AND SOURCE OF CONTAGION is the human being and the transmission is through SEXUAL RELATIONS and eventually BLOOD TRANSFUSIONS of contaminated people. The source of LYME DISEASE CONTAGION are TICKS and there are many animals that act as hosts between them DEER, BIRDS, and MICE, also DNA sequences of BORRELIA have been found in domestic animals such as DOGS, CATS AND HORSES.
E.) Both ESPIROCHETES can be detected by blood tests:
- SYPHILIS: VDRL, PCR, Enzyme Immunoassay (IEA), FTA ABs.
- LYME: Western Blot (IgG, IgM, Multiplex PCR, enzyme-linked immunosorbent assay (ELISA), enzyme immunoassay (IEA), indirect immunofluorescence IGg and IgM). IgA / IgG / IgM IFA Screen, Immunoblot IgM, IgG, IGXspot, IgM, IgG 31 Kda Epitope test.
F.) ANOTHER BIG DIFFERENCE BETWEEN BOTH is that today, after the PENICILLINE WAS DISCOVERED, it is still the first OPTION in SYPHILIS and the TREPONEMA PALLIDUM has not generated ANTIBIOTIC RESISTANCE, also the DOXYCYCLIN and TETRACYCLINE are effective in the disease. Another detail is that although the TREPONEMA presents other species, only the TREPONEMA PALLIDUM PALLIDUM is the causal agent of SYPHILIS.
G.) In the case of LYME DISEASE there are many SPECIES OF BORRELIA that have been described in the different geographical areas of the world that cause this disease, having described more than 52 species in total. Of which 21 species are already recognized and distributed throughout the world:
Of these: 10 species are pathogenic for humans, they are: B. afzelii, B. bavariensis, B. bissettii, B. burgdorferi sensu stricto, B. garinii, B. kurtenbachii, B. lusitaniae, B. mayonii, B. spielmanii, B. valaisiana, not to mention the Borrelia Miyamitoi causing the RECURRENT FEVER described in the year 1.994 and which in 2.011 was described in Human in Russia; United States, Japan and Europe.
Of these, there are eleven (11) identified species that have not yet been detected or isolated from humans. This group includes B. americana, B. andersonii, B. californiensis, B. carolinensis, B. chilensis, B. finlandensis, B. japonica, B. tanukii, B. turdi, B. sinica and B. yangtze.
H.) LYME and SYPHILIS share 3 clinical stages: PRIMARY, SECONDARY and LATE (NEUROBORRELIOSIS AND NEUROSYPHILIS)
LEPROSY AND LYME'S DISEASE:
===========================
A.) Both diseases or pests are mentioned in the BIBLE.
B.) LEPROSY is not transmitted from pregnant women to the Fetus; in the LYME DISEASE this transmission has been described.
C.) Like SYPHILIS, for LEPRA there is only one causal agent described by Armauer Hansen in 1.783, MYCOBACTERIUM LEPRA, and 225 years later, year 2.008, a sub-species named MYCOBATERIUM LEPROMATOSIS was described. Unlike the disease of LYME that as described above, causal agent BORRELIA BURGORFERI, it has many species that affect humans.
D.) LEPROSY is highly contagious from HUMAN TO HUMAN, mainly through nasal secretion, the main mechanism of dissemination, and as natural reservoirs, the nine-banded Armadillo (Dasypus novemcinctus, Mycobacterium Leprae) and the Red squirrels (Mycobacterium Lepromatosis), in the British Islands is described, but I repeat this ancestral disease has MAN as its principal HOST and source of CONTAGION.
However, in the Southeast of the United States in the year 2015, several cases of transmission of nine-(9) banded Armadillos to humans were described, so it is also considered a zoonotic disease.
The LYME DISEASE is not transmitted from HUMAN-HUMAN, the main VECTOR are TICKS and its majority RESERVORIES are the animals already described. One of the big differences between these two (2) pests.
E.) The diagnosis of THE LEPROSY is done by:
- CLINICALLY: type of lesions
- LYMPHA exam: Giemsa coloration.
- SKIN Biopsy: Hematoxylin Eosin (HE) and Faraco-Fite coloration.
- GEOGRAPHIC Distribution: Endemic areas.
- LABORATORY tests: PCR.
As I said before the diagnosis of LYME disease apart from the clinical manifestations, it is made based on laboratory tests MANY OF WHICH result in "NEGATIVE" being positive patients. In the BIOPSIES of the skin lesions in which the diagnosis is suspected and confirmed by laboratory diagnosis BORRELIA IS NOT DETECTED in the majority of cases except for THE BORRELIAL LYMPHOCYTOMA where in skin biopsy this causative agent has been found. In the skin biopsies of the LEPROSY NODULES, in 100% you find the Mycobaterium Leprae.
E.) THE MYCOBACTERIUM LEPRAE has never been cultivated. With the BORRELIA BURGDROFERI it has been done.
F.) The tremendous LEPROSY pest has been dominated and diminished NOTABLY the cases in the world with the MULTI-DRUGS THERAPY: DAPSONE (SULFA), + CLOFAZIMINE + RIFAMIPICIN, in combination with others that already mention: OFLOXACIN, MINOCYCLINE, CLARITHROMYCIN, and AMOXICILLIN. Cases of LEPROSY resistant to classical treatment of (MTD) and other antimicrobials have been described. With the LYME DISEASE, exactly the same thing occurs, but to a greater degree, probably due to the numerous species of the BORRELIA that cause the disease.
In LYME disease, the treatment schemes already mentioned in HANSEN disease or LEPROSY have been used very little.
THE MISSING LINKS:
==================
1.) CONFIRMATION OF THE DIAGNOSIS:
================================
As you can see, this is one of the GREAT DIFFERENCES between SYPHILIS, LEPROSY AND LYME: THE SEROLOGICAL DIAGNOSIS, in SYPHILIS, is HIGHLY PRECISE, in the LYME DISEASE, the CDC only approves 2 types of tests and many of them result in "NEGATIVE", and often after other tests is that the patient is "POSITIVE" perhaps when the disease has already damaged your body. In the case of LEPROSY also the diagnosis of the disease is more than 90% I would say in its entirety, it is also PRECISE AND EXACT This is one of the major problems that is causing at the level of public health is in LYME disease: THE CONFIRMATION OF THE DIAGNOSIS.
2.) EFFECTIVENESS OF TREATMENT:
===============================
As I said above, the SYPHILIS today, after 74 years of being used PENICILLIN, to treat this disease it is still the FIRST OPTION, followed by others like doxycycline and tetracyclines. This means that the TREPONEMA PALLIDUM has not developed resistance to this NOBLE ANTIBIOTIC.
In the case of Leprosy the TRIPLE COMBINATION of DAPSONE + CLOFAZIMIN + RIFAMPICIN, for years was the mainstay of the treatment of the disease to the point that this fact was the one that decreed (I have said several times) the closure of LEPROSERIES in the world. Afterwards, resistance to these drugs appeared, but others appeared, to help the treatment such as MINOCYCLINE OFLOXACIN and others.
On the contrary, in the case of LYME DISEASE, BORRELIA, and its multiple species is well known as having developed RESISTANCE to many antibiotics, including DOXYCYCLINE, TETRACYCLINES, AMOXICILIN, PENICILLINE and others considered highly effective against it, this fact being one of the GREAT CHALLENGES today against this plague today.
3.) RESISTANCE TO TREATMENT:
==========================
1.) In the SIFILIS, practically there is no resistance to BENZATHINE PENICILLIN G. and others used, since the TREPONEMA PALLIDUM PALLIDUM, has not offered mutations. It remains the same.
2.) In LEPROSY, it occurs almost the same as SIYPHILIS, Mycobacterium Leprae has not mutated, and 225 years passed for the sub-species to be described: Mycobacterium Lepromatosis, in 2.008. Therefore the CLASSIC TREATMENT Multy drug Therapy is still valid (DAPSONE + CLOFAZIMINE + RIFAMPICIN) with variations in the cases of resistance that were described years later, where the MINOCYCLINE is included as first alternative in help.
3.) In the case of LYME disease, the story is another the BORRELIA BURDORGFERI and its species have developed RESISTANCE to almost all existing treatments, which I have already described in my previous publications. THE CODES OF THE LYME DISEASE. I AND II
CONCLUSIONS:
=============
Maybe you're asking why I made this triple comparison: LYME, LEPROSY, AND SYPHILIS, and as always I'll give you the answer.
1.) They are diseases described in the BIBLE as "PESTS" or evils sent by God to the human being, ancestral diseases and APOCALIPTICS.
2.) Even having discovered its causal agents and treatments: these plagues LYME SYPHILIS and LEPROSY continue to exist in the whole world.
3.) The SYPHILIS and LEPROSY show still a high sensitivity to the KNOWN treatments.
4.) LYME, is the one that presents greater difficulty in diagnosis SEROLOGIC and TREATMENT for the development of resistance and the "ability" of this Spirochete to "evade" the diagnostic tests.
5.) In the present review I see that DAPSONE or DIAMINODIPHENYLSULFONE (DDS) drug that has practically killed LEPROSY is not being used frequently in LYME disease, they have dismissed its use, having described the SENSITIVITY OF BORRELIA to this drug . End of story:
DAPSONE + CLOFAZIMINE + RIFAMPICIN, or DAPSONE + MINOCYCLINE + CLOFAZIMINE must be used in the LYME disease.
BIBLICAL words.
Greetings to all.
Dr. Jose Lapenta.
===============
If you think that the LYME disease was discovered in 1.981 when Wllly Burgdorfer described the causative agent of this disease, the ESPIROCHETE BORRELIA, whose name is BURGDORFERI in honor of the discoverer, you are wrong.
The TICKS as a plague are also described in the HOLY BIBLE, in THE BOOK OF EXODUS, reference is made to the plagues that God would send to the Pharaoh of Egypt, and among them are frogs, horsefly, lobsters, lice and mosquitoes .... "
"... And the dust of the earth became lice throughout the land of Egypt" ... a well-knowledgeable tourist from Egypt observed that the sand seemed to move; observing more closely, he saw that the surface of the earth was a mass of tiny ticks ... "
The first descriptions of LYME DISEASE date from the post-colonial era in New England: geographic region comprising six states of the Northeast of the United States: Maine, Vermont, New Hampshire, Massachusetts, Rhode Island and Connecticut, and from there I later disseminated to the Midwest.
The first descriptions date from the years 1,663 to 1,670, in New England, by John Josselyn, later in 1.749, Peter Kalm Swedish botanist in the forests of New York. 100 years later, the forests had disappeared and the Lyme bacteria had probably been isolated in some outbreaks along the northeast coast, Wisconsin and Minnesota.
But the first description of the most accurate LYME DISEASE dates from the year 1.764 by the Reverend John Walker on the Isle of Jura (Island of the Deer) in Scotland. Many people from this area of Great Britain emigrated to North America from the year 1.717.
BORRELIA DNA was found in an IXODES RICINUS TICKS in Germany dating from the year 1.884, in an infected mouse that died in 1.894, and beyond this in the autopsy of the Ötzi Mummy "Ice Man" (5,300 years) in the year 2.010 was found DNA sequences of BORRELIA BURGDORFERI, proof that it is a BIBLICAL pest, this mummy become the oldest human with LYME DISEASE.
The word LYME comes from a town in Connecticut that bears that name where the first cases described as ARTHRITIS OF LYME appeared, or ERYTHEMA MIGRANS.
THE SYPHILIS:
============
Sexually transmitted diseases SYPHILIS AND GONORRHEA, are also mentioned in the BIBLE, in the book GENESIS: 12, which refers to SARA, wife of ABRAHAM infected with a sexually transmitted disease, which later spread to the court of Pharaoh and his concubines; also in the LEVITICUS, Old Testament chapter 15 says the following”
"... Moses and Aaron received from Yahweh on this point:" Speak to the children of Israel and say to them, "Any man who has a seminal discharge in his flesh will be unclean." This is the law of his uncleanness in the flow, either because his flesh distills the flow, or by holding it in. It is unclean ... "They were probably referring to these two diseases, which were later described as separate entities.
The exact origin of the SYPHILIS is in dispute. It is said that there are two theories, one pre-Columbian, that locates it in Europe before the trip of Christopher Columbus to the Americas, and another Columbine, associated with his trip to the Americas, where he was taken to Europe by the infected crew.
In 1.530 it was that the term "SYPHILIS" was used for the first time by the Italian doctor and poet Girolamo Fracastoro, and REFERS to the character of a work, called: " Syphilis or the French disease "who refers to a character called SYPHILUS , punished by the gods to suffer a terrible disease. The poem deals with the ravages of the disease in ITALY at that time, specifically in the city of Naples in the years 1,944 and 1.945, during the French invasion.
The causal agent TREPONEMA PALLIDUM is an ESPIROCHETE as well as LYME DISEASE and was discovered by Fritz Schaudinn and Erich Hoffmann in 1.905. In 1.910 the first treatment for SYPHILIS named Salvarsan, (arsphenamine or compound 606) by German Paul Erlich, a derivative of arsenic, who won him the Nobel Prize for Medicine, and which was popularized with the name "MAGIC BULLET".
Subsequently, the mercurial salts were used from 1.912, then Bismuth from 1.922. The QUININE treatment for malaria was also used in the tertiary syphilis or NEUROSYPHILIS and this treatment won him the Nobel Prize for medicine to Julius Wagner-Jauregg in 1.927.
IN 1.928 appears the noble PENICILLINE discovered by ALEXANDER FLEMING, which began to be used in the SYPHILIS in 1.943, being today STILL the first choice of treatment for this disease.
It is said that famous people like: Franz Schubert, Al Capone and Édouard Manet had the disease.
THE WORD SYPHILIS comes from LATIN: SIPH: PIG. PHILUS: LOVE
THE SYPHILIS AND LYME'S DISEASE:
==============================
A.) Both diseases are produced by ESPIROCHETES, in the case of the SYPHILIS, the TREPONEMA PALLIDUM PALLIDUM, in the case of LYME the BORRELIA BURGDORFERI.
B.) Both diseases can be transmitted in pregnant women to the FETUS.
C.) Both ESPIROHETES can be detected by OPTIC MICROSCOPY, "Dark Field" in SYPHILIS and "Blue Color staining" (Professor Laane and Ivar Mysterud).
D.) There are no natural HOSTS for the SYPHILIS, the main RESERVOIR AND SOURCE OF CONTAGION is the human being and the transmission is through SEXUAL RELATIONS and eventually BLOOD TRANSFUSIONS of contaminated people. The source of LYME DISEASE CONTAGION are TICKS and there are many animals that act as hosts between them DEER, BIRDS, and MICE, also DNA sequences of BORRELIA have been found in domestic animals such as DOGS, CATS AND HORSES.
E.) Both ESPIROCHETES can be detected by blood tests:
- SYPHILIS: VDRL, PCR, Enzyme Immunoassay (IEA), FTA ABs.
- LYME: Western Blot (IgG, IgM, Multiplex PCR, enzyme-linked immunosorbent assay (ELISA), enzyme immunoassay (IEA), indirect immunofluorescence IGg and IgM). IgA / IgG / IgM IFA Screen, Immunoblot IgM, IgG, IGXspot, IgM, IgG 31 Kda Epitope test.
F.) ANOTHER BIG DIFFERENCE BETWEEN BOTH is that today, after the PENICILLINE WAS DISCOVERED, it is still the first OPTION in SYPHILIS and the TREPONEMA PALLIDUM has not generated ANTIBIOTIC RESISTANCE, also the DOXYCYCLIN and TETRACYCLINE are effective in the disease. Another detail is that although the TREPONEMA presents other species, only the TREPONEMA PALLIDUM PALLIDUM is the causal agent of SYPHILIS.
G.) In the case of LYME DISEASE there are many SPECIES OF BORRELIA that have been described in the different geographical areas of the world that cause this disease, having described more than 52 species in total. Of which 21 species are already recognized and distributed throughout the world:
Of these: 10 species are pathogenic for humans, they are: B. afzelii, B. bavariensis, B. bissettii, B. burgdorferi sensu stricto, B. garinii, B. kurtenbachii, B. lusitaniae, B. mayonii, B. spielmanii, B. valaisiana, not to mention the Borrelia Miyamitoi causing the RECURRENT FEVER described in the year 1.994 and which in 2.011 was described in Human in Russia; United States, Japan and Europe.
Of these, there are eleven (11) identified species that have not yet been detected or isolated from humans. This group includes B. americana, B. andersonii, B. californiensis, B. carolinensis, B. chilensis, B. finlandensis, B. japonica, B. tanukii, B. turdi, B. sinica and B. yangtze.
H.) LYME and SYPHILIS share 3 clinical stages: PRIMARY, SECONDARY and LATE (NEUROBORRELIOSIS AND NEUROSYPHILIS)
LEPROSY AND LYME'S DISEASE:
===========================
A.) Both diseases or pests are mentioned in the BIBLE.
B.) LEPROSY is not transmitted from pregnant women to the Fetus; in the LYME DISEASE this transmission has been described.
C.) Like SYPHILIS, for LEPRA there is only one causal agent described by Armauer Hansen in 1.783, MYCOBACTERIUM LEPRA, and 225 years later, year 2.008, a sub-species named MYCOBATERIUM LEPROMATOSIS was described. Unlike the disease of LYME that as described above, causal agent BORRELIA BURGORFERI, it has many species that affect humans.
D.) LEPROSY is highly contagious from HUMAN TO HUMAN, mainly through nasal secretion, the main mechanism of dissemination, and as natural reservoirs, the nine-banded Armadillo (Dasypus novemcinctus, Mycobacterium Leprae) and the Red squirrels (Mycobacterium Lepromatosis), in the British Islands is described, but I repeat this ancestral disease has MAN as its principal HOST and source of CONTAGION.
However, in the Southeast of the United States in the year 2015, several cases of transmission of nine-(9) banded Armadillos to humans were described, so it is also considered a zoonotic disease.
The LYME DISEASE is not transmitted from HUMAN-HUMAN, the main VECTOR are TICKS and its majority RESERVORIES are the animals already described. One of the big differences between these two (2) pests.
E.) The diagnosis of THE LEPROSY is done by:
- CLINICALLY: type of lesions
- LYMPHA exam: Giemsa coloration.
- SKIN Biopsy: Hematoxylin Eosin (HE) and Faraco-Fite coloration.
- GEOGRAPHIC Distribution: Endemic areas.
- LABORATORY tests: PCR.
As I said before the diagnosis of LYME disease apart from the clinical manifestations, it is made based on laboratory tests MANY OF WHICH result in "NEGATIVE" being positive patients. In the BIOPSIES of the skin lesions in which the diagnosis is suspected and confirmed by laboratory diagnosis BORRELIA IS NOT DETECTED in the majority of cases except for THE BORRELIAL LYMPHOCYTOMA where in skin biopsy this causative agent has been found. In the skin biopsies of the LEPROSY NODULES, in 100% you find the Mycobaterium Leprae.
E.) THE MYCOBACTERIUM LEPRAE has never been cultivated. With the BORRELIA BURGDROFERI it has been done.
F.) The tremendous LEPROSY pest has been dominated and diminished NOTABLY the cases in the world with the MULTI-DRUGS THERAPY: DAPSONE (SULFA), + CLOFAZIMINE + RIFAMIPICIN, in combination with others that already mention: OFLOXACIN, MINOCYCLINE, CLARITHROMYCIN, and AMOXICILLIN. Cases of LEPROSY resistant to classical treatment of (MTD) and other antimicrobials have been described. With the LYME DISEASE, exactly the same thing occurs, but to a greater degree, probably due to the numerous species of the BORRELIA that cause the disease.
In LYME disease, the treatment schemes already mentioned in HANSEN disease or LEPROSY have been used very little.
THE MISSING LINKS:
==================
1.) CONFIRMATION OF THE DIAGNOSIS:
================================
As you can see, this is one of the GREAT DIFFERENCES between SYPHILIS, LEPROSY AND LYME: THE SEROLOGICAL DIAGNOSIS, in SYPHILIS, is HIGHLY PRECISE, in the LYME DISEASE, the CDC only approves 2 types of tests and many of them result in "NEGATIVE", and often after other tests is that the patient is "POSITIVE" perhaps when the disease has already damaged your body. In the case of LEPROSY also the diagnosis of the disease is more than 90% I would say in its entirety, it is also PRECISE AND EXACT This is one of the major problems that is causing at the level of public health is in LYME disease: THE CONFIRMATION OF THE DIAGNOSIS.
2.) EFFECTIVENESS OF TREATMENT:
===============================
As I said above, the SYPHILIS today, after 74 years of being used PENICILLIN, to treat this disease it is still the FIRST OPTION, followed by others like doxycycline and tetracyclines. This means that the TREPONEMA PALLIDUM has not developed resistance to this NOBLE ANTIBIOTIC.
In the case of Leprosy the TRIPLE COMBINATION of DAPSONE + CLOFAZIMIN + RIFAMPICIN, for years was the mainstay of the treatment of the disease to the point that this fact was the one that decreed (I have said several times) the closure of LEPROSERIES in the world. Afterwards, resistance to these drugs appeared, but others appeared, to help the treatment such as MINOCYCLINE OFLOXACIN and others.
On the contrary, in the case of LYME DISEASE, BORRELIA, and its multiple species is well known as having developed RESISTANCE to many antibiotics, including DOXYCYCLINE, TETRACYCLINES, AMOXICILIN, PENICILLINE and others considered highly effective against it, this fact being one of the GREAT CHALLENGES today against this plague today.
3.) RESISTANCE TO TREATMENT:
==========================
1.) In the SIFILIS, practically there is no resistance to BENZATHINE PENICILLIN G. and others used, since the TREPONEMA PALLIDUM PALLIDUM, has not offered mutations. It remains the same.
2.) In LEPROSY, it occurs almost the same as SIYPHILIS, Mycobacterium Leprae has not mutated, and 225 years passed for the sub-species to be described: Mycobacterium Lepromatosis, in 2.008. Therefore the CLASSIC TREATMENT Multy drug Therapy is still valid (DAPSONE + CLOFAZIMINE + RIFAMPICIN) with variations in the cases of resistance that were described years later, where the MINOCYCLINE is included as first alternative in help.
3.) In the case of LYME disease, the story is another the BORRELIA BURDORGFERI and its species have developed RESISTANCE to almost all existing treatments, which I have already described in my previous publications. THE CODES OF THE LYME DISEASE. I AND II
CONCLUSIONS:
=============
Maybe you're asking why I made this triple comparison: LYME, LEPROSY, AND SYPHILIS, and as always I'll give you the answer.
1.) They are diseases described in the BIBLE as "PESTS" or evils sent by God to the human being, ancestral diseases and APOCALIPTICS.
2.) Even having discovered its causal agents and treatments: these plagues LYME SYPHILIS and LEPROSY continue to exist in the whole world.
3.) The SYPHILIS and LEPROSY show still a high sensitivity to the KNOWN treatments.
4.) LYME, is the one that presents greater difficulty in diagnosis SEROLOGIC and TREATMENT for the development of resistance and the "ability" of this Spirochete to "evade" the diagnostic tests.
5.) In the present review I see that DAPSONE or DIAMINODIPHENYLSULFONE (DDS) drug that has practically killed LEPROSY is not being used frequently in LYME disease, they have dismissed its use, having described the SENSITIVITY OF BORRELIA to this drug . End of story:
DAPSONE + CLOFAZIMINE + RIFAMPICIN, or DAPSONE + MINOCYCLINE + CLOFAZIMINE must be used in the LYME disease.
"... Everything you will take from the earth, the earth will return it to you, if you do not help your neighbor, crushed by any plague, soon the plagues will turn against you, your neighbor will be free and you will live the chains that those lived ... "
BIBLICAL words.
Greetings to all.
Dr. Jose Lapenta.
Dr. Jose M. Lapenta.
=====================================================================
REFERENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
=====================================================================
1.) Activity of Sulfa Drugs and Their Combinations against Stationary Phase B. burgdorferi In Vitro. Antibiotics (Basel). 2017 Mar 22;6(1). pii: E10. doi: 10.3390/antibiotics6010010. [PUBMED]
Feng J1, Zhang S2, Shi W3, Zhang Y4.
2.) The Use of Dapsone as a Novel “Persister” Drug in the Treatment of Chronic
Lyme Disease/Post Treatment Lyme Disease Syndrome. Richard I Horowitz, MD and Phyllis Freeman, PhD. Hudson Valley Healing Arts Center, New York, USA
3.) Identification of novel activity against Borrelia burgdorferi persisters using an FDA approved drug library. Emerg Microbes Infect. 2014 Jul;3(7):e49. doi: 10.1038/emi.2014.53. Epub 2014 Jul 2. [PUBMED] Feng J1, Wang T1, Shi W1, Zhang S1, Sullivan D1, Auwaerter PG2, Zhang Y1.
4.) A Drug Combination Screen Identifies Drugs Active against Amoxicillin-Induced Round Bodies of In Vitro Borrelia burgdorferi Persisters from an FDA Drug Library. Front Microbiol. 2016 May 23;7:743. doi: 10.3389/fmicb.2016.00743. eCollection 2016. [PUBMED] Feng J1, Shi W1, Zhang S1, Sullivan D1, Auwaerter PG2, Zhang Y1.
5.) In vitro susceptibility of Borrelia burgdorferi isolates to three antibiotics commonly used for treating equine Lyme disease. BMC Vet Res. 2017 Sep 29;13(1):293. doi: 10.1186/s12917-017-1212-3. [PUBMED] Caol S1,2, Divers T3, Crisman M4, Chang YF1.
6.) Enfermedad de Lyme crónica y coinfecciones : diagnóstico diferencial. Open Neurol J. 2012; 6: 158-78. doi: 10.2174 / 1874205X01206010158. Epub 2012 28 de diciembre. [PUBMED]Berghoff W 1 .
7.) In vitro and in vivo antibiotic susceptibility of Lyme disease Borrelia isolated from the ixodid tick in Japan. J Dermatol. 1995 Dec;22(12):935-8. [PUBMED] Fujita H1, Yamada K, Kurita T, Masuzawa T, Yanagihara Y.
8.) Minocycline in lepromatous leprosy. Int J Lepr Other Mycobact Dis, 63(1):8-17 1995 Mar
[PUBMED] Fajardo TT Jr; Villahermosa LG; dela Cruz EC; Abalos RM; Franzblau SG; Walsh GP
9.) Efficacy of minocycline in single dose and at 100 mg twice daily for lepromatous leprosy. Int J Lepr Other Mycobact Dis (United States), Dec 1994, 62(4) p568-73 . Gelber RH; Murray LP; Siu P; Tsang M; Rea AUTHOR'S ADDRESS: San Francisco Regional Hansen's Disease Program, CA 94115.
10.) Field trial on efficacy of supervised monthly dose of 600 mg rifampin, 400 mg ofloxacin and 100 mg minocycline for the treatment of leprosy; first results. Int J Lepr Other Mycobact Dis, 65(2):224-9 1997 Jun. Mane I; Cartel JL; Grosset JH
11.) Bactericidal activity of a single-dose combination of ofloxacin plus minocycline, with or without rifampin, against Mycobacterium leprae in mice and in lepromatous patients. Antimicrob Agents Chemother, 42(5):1115-20 1998 May. [PUBMED] Ji B; Sow S; Perani E; Lienhardt C; Diderot V; Grosset J
12.)Efficacy of single dose multidrug therapy for the treatment of single-lesion paucibacillary leprosy. Single-lesion Multicentre Trial Group. Indian J Lepr, 69(2):121-9 1997 Apr-Jun [PUBMED] no author listed.
13.) Bactericidal activity of single dose of clarithromycin plus minocycline, with or without ofloxacin, against Mycobacterium leprae in patients. Antimicrob Agents Chemother, 40(9):2137-41 1996 Sep [PUBMED] Ji B; Jamet P; Perani EG; Sow S; Lienhardt C; Petinon C; Grosset JH
14.) Chronic Lyme borreliosis at the root of multiple sclerosis--is a cure with antibiotics attainable? Med Hypotheses. 2005;64(3):438-48. [PUBMED] Fritzsche M1.
15.) Hansen's Disease and Rheumatoid Arthritis Crossover of Clinical Symptoms: A Case Series of 18 Patients in the United States. Am J Trop Med Hyg. 2017 Dec;97(6):1726-1730. doi: 10.4269/ajtmh.17-0197. Epub 2017 Oct 19. [PUBMED] Labuda SM1, Schieffelin JS1, Shaffer JG2, Stryjewska BM3.
16.) Leprosy - an overview of clinical features, diagnosis, and treatment. J Dtsch Dermatol Ges. 2017 Aug;15(8):801-827. doi: 10.1111/ddg.13301. [PUBMED] Fischer M1.
17.) Multidrug therapy for leprosy: a game changer on the path to elimination. Lancet Infect Dis. 2017 Sep;17(9):e293-e297. doi: 10.1016/S1473-3099(17)30418-8. Epub 2017 Jul 7. [PUBMED]Smith CS1, Aerts A2, Saunderson P3, Kawuma J4, Kita E5, Virmond M6.
18.) Infectious neuropathies. Neurol Clin. 2007 Feb;25(1):115-37. [PUBMED] Said G1.
19.) A case presentation of bilateral simultaneous Bell's palsy. Am J Otolaryngol. 2003 Jul-Aug;24(4):271-3. [PUBMED] Kilic R1, Ozdek A, Felek S, Safak MA, Samim E.
20.) Inflammatory neuropathies associated with known infections (HIV, leprosy, Chagas' disease, Lyme disease). Baillieres Clin Neurol. 1994 Apr;3(1):149-71. [PUBMED] Said G1.
21.) Antibiotic-refractory Lyme arthritis is associated with HLA-DR molecules that bind a Borrelia
burgdorferi peptide. J Exp Med. 2006 Apr 17;203(4):961-71. Epub 2006 Apr 3. [PUBMED] Steere AC1, Klitz W, Drouin EE, Falk BA, Kwok WW, Nepom GT, Baxter-Lowe LA.
22.) HLA-DR alleles determine responsiveness to Borrelia burgdorferi antigens in a mouse model of self-perpetuating arthritis. Arthritis Rheum. 2009 Dec;60(12):3831-40. doi: 10.1002/art.25005.
[PUBMED] Iliopoulou BP1, Guerau-de-Arellano M, Huber BT.
23.) Association of treatment-resistant chronic Lyme arthritis with HLA-DR4 and antibody reactivity to OspA and OspB of Borrelia burgdorferi. Infect Immun. 1993 Jul;61(7):2774-9. [PUBMED] Kalish RA1, Leong JM, Steere AC.
24.) HLA-B*13:01 and the dapsone hypersensitivity syndrome. N Engl J Med. 2013 Oct 24;369(17):1620-8. doi: 10.1056/NEJMoa1213096. [PUBMED] Zhang FR1, Liu H, Irwanto A, Fu XA, Li Y, Yu GQ, Yu YX, Chen MF, Low HQ, Li JH, Bao FF, Foo JN, Bei JX, Jia XM, Liu J, Liany H, Wang N, Niu GY, Wang ZZ, Shi BQ, Tian HQ, Liu HX, Ma SS, Zhou Y, You JB, Yang Q, Wang C, Chu TS, Liu DC, Yu XL, Sun YH, Ning Y, Wei ZH, Chen SL, Chen XC, Zhang ZX, Liu YX, Pulit SL, Wu WB, Zheng ZY, Yang RD, Long H, Liu ZS, Wang JQ, Li M, Zhang LH, Wang H, Wang LM, Xiao P, Li JL, Huang ZM, Huang JX, Li Z, Liu J, Xiong L, Yang J, Wang XD, Yu DB, Lu XM, Zhou GZ, Yan LB, Shen JP, Zhang GC, Zeng YX, de Bakker PI, Chen SM, Liu JJ.
25.) Increase in the incidence of dapsone hypersensitivity syndrome--an appraisal. Lepr Rev. 2001 Mar;72(1):57-62. [PUBMED] Rao PN1, Lakshmi TS.
26.) Associations of HLA DR and DQ molecules with Lyme borreliosis in Latvian patients. BMC Res Notes. 2012 Aug 14;5:438. doi: 10.1186/1756-0500-5-438. [PUBMED] Kovalchuka L1, Eglite J, Lucenko I, Zalite M, Viksna L, Krumiņa A.
27.) Minocycline hepatotoxicity: Clinical characterization and identification of HLA-B∗35:02 as a risk factor. J Hepatol. 2017 Jul;67(1):137-144. doi: 10.1016/j.jhep.2017.03.010. Epub 2017 Mar 18. [PUBMED] Urban TJ1, Nicoletti P2, Chalasani N3, Serrano J4, Stolz A5, Daly AK6, Aithal GP7, Dillon J8, Navarro V9, Odin J10, Barnhart H11, Ostrov D12, Long N1, Cirulli ET11, Watkins PB1, Fontana RJ13; Drug-Induced Liver Injury Network (DILIN); Pharmacogenetics of Drug-Induced Liver Injury group (DILIGEN); International Serious Adverse Events Consortium (iSAEC).
28.) Advances in Serodiagnostic Testing for Lyme Disease Are at Hand. Clin Infect Dis. 2017 Dec 7. doi: 10.1093/cid/cix943. [Epub ahead of print] [PUBMED] Branda JA1, Body BA2, Boyle J3, Branson BM4, Dattwyler RJ5, Fikrig E6, Gerald NJ7, Gomes-Solecki M8, Kintrup M9, Ledizet M10, Levin AE11, Lewinski M12, Liotta LA13, Marques A14, Mead PS15, Mongodin EF16, Pillai S17, Rao P7, Robinson WH18, Roth KM7, Schriefer ME15, Slezak T19, Snyder J20, Steere AC21, Witkowski J22, Wong SJ23, Schutzer SE24.
29.) Hall, Stephen S (November 2011). "Iceman Autopsy". National Geographic. Archived from the original on 19 October 2011. Retrieved 17 October 2011.
30.) Josselyn, John (1670). An Account of Two Voyages to New-England Made during the Years 1638, 1663. Archived from the original on 25 June 2013.page 92
31.) Hoen AG, Margos G, Bent SJ, et al. (September 2009). "Phylogeography of Borrelia burgdorferi in the eastern United States reflects multiple independent Lyme disease emergence events". Proc. Natl. Acad. Sci. U.S.A. 106 (35): 15013–18. Bibcode:2009PNAS..10615013H. doi:10.1073/pnas.0903810106. JSTOR 40484546. PMC 2727481 Freely accessible. PMID 19706476. Lay summary – YaleNews (10 August 2009).
32.) Drymon, MM (2008). Disguised as the devil: how Lyme disease created witches and changed history. pp. 51–52. ISBN 978-0-615-20061-3.
33.) Summerton N (1995). "Lyme disease in the eighteenth century". BMJ. 311 (7018): 1478. doi:10.1136/bmj.311.7018.1478.
34.) Holy bible: Genesis: 12; Exodus: 8: 6-9: 7; Leviticus, 13:12, Leviticus: 15
35.) Harper, KN; Zuckerman, MK; Harper, ML; Kingston, JD; Armelagos, GJ (2011). "The origin and antiquity of syphilis revisited: an appraisal of Old World pre-Columbian evidence for treponemal infection". American Journal of Physical Anthropology. 146 Suppl 53: 99–133. doi:10.1002/ajpa.21613. PMID 22101689.
36.) Winters, Adam (2006). Syphilis. New York: Rosen Pub. Group. p. 17. ISBN 9781404209060. Archived from the original on 4 March 2016.
37.) Dormandy, Thomas (2006). The worst of evils: man's fight against pain: a history (Uncorrected page proof. ed.). New Haven: Yale University Press. p. 99. ISBN 978-0300113228.
38.) Anthony Grafton (March 1995). "Drugs and Diseases: New World Biology and Old World Learning". New Worlds, Ancient Texts The Power of Tradition and the Shock of Discovery. Harvard University Press. pp. 159–194. ISBN 9780674618763.
39.) Identification of the leprosy agent Mycobacterium lepromatosis in Singapore.
J Drugs Dermatol. 2012 Feb;11(2):168-72. [PUBMED] Han XY1, Sizer KC, Tan HH.
40.) Mutations in the drug resistance-determining region of Mycobacterium lepromatosis isolated from leprosy patients in Mexico. J Dermatol. 2016 Nov;43(11):1345-1349. doi: 10.1111/1346-8138.13483. Epub 2016 Jun 27. [PUBMED] Kai M1, Fafutis-Morris M2, Miyamoto Y3, Mukai T3, Mayorga-Rodriguez J2, Rodriguez-Castellanos MA2, Martínez-Guzman MA2, Matsuoka M3.
41.) Farhi, D; Dupin, N (Sep–Oct 2010). "Origins of syphilis and management in the immunocompetent patient: facts and controversies". Clinics in dermatology. 28 (5): 533–8. doi:10.1016/j.clindermatol.2010.03.011. PMID 20797514.
42.) Franzen, C (December 2008). "Syphilis in composers and musicians--Mozart, Beethoven, Paganini, Schubert, Schumann, Smetana". European Journal of Clinical Microbiology & Infectious Diseases. 27 (12): 1151–7. doi:10.1007/s10096-008-0571-x. PMID 18592279.
43.) Fracastor, Hieronymus (1911). Syphilis. The Philmar Company. "Syphilis". Online Etymology Dictionary. 2001.
44.) Raju T (2006). "Hot brains: manipulating body heat to save the brain" (PDF). Pediatrics. 117 (2): e320–1.
45.) Early syphilis: serological treatment response to doxycycline/tetracycline versus benzathine penicillin. J Infect Dev Ctries. 2014 Feb 13;8(2):228-32. doi: 10.3855/jidc.3013. [PUBMED] . Li J1, Zheng HY.
46.) Surveillance for Borrelia burgdorferi in Ixodes Ticks and Small Rodents in British Columbia.
Vector Borne Zoonotic Dis. 2015 Nov;15(11):701-5. doi: 10.1089/vbz.2015.1854. Epub 2015 Oct 26. [PUBMED] Morshed MG1,2, Lee MK1, Man S1, Fernando K1, Wong Q1, Hojgaard A3, Tang P1,2, Mak S4, Henry B2,5, Patrick DM2,4.
47.) Borrelia miyamotoi Infections in Humans and Ticks, Northeastern China. Emerg Infect Dis. 2018 Feb;24(2):236-241. doi: 10.3201/eid2402.160378. [PUBMED] Jiang BG, Jia N, Jiang JF, Zheng YC, Chu YL, Jiang RR, Wang YW, Liu HB, Wei R, Zhang WH, Li Y, Xu XW, Ye JL, Yao NN, Liu XJ, Huo QB, Sun Y, Song JL, Liu W, Cao WC.
48.) A simple method for the detection of live Borrelia spirochaetes in human blood using classical microscopy techniques. Morten Motzfeldt Laane, Ivar Mysterud. Published 2013. Semantic Sholar. Source: https://www.semanticscholar.org/paper/A-simple-method-for-the-detection-of-live-Borrelia-Laane-Mysterud/4f6251e40f196b094905d84e87b8b6fe8d1d1636
49.) Pustular secondary syphilis: report of three cases and review of the literature. Int J Dermatol. 2014 Oct;53(10):e428-31. doi: 10.1111/ijd.12337. Epub 2014 Sep 10. [PUBMED]Kazlouskaya V1, Wittmann C, Tsikhanouskaya I.
50.) Serological Evidence of Borrelia Burgdorferi Infection in Mexican Patients with Facial Palsy. Rev Invest Clin. 2017 Nov-Dec;69(6):344-348. doi: 10.24875/RIC.17002344. [PUBMED] Gordillo-Pérez G1, García-Juárez I1, Solórzano-Santos F2, Corrales-Zúñiga L3, Muñoz-Hernández O2, Torres-López J1.
51.) Polymerase chain reaction in diagnosis of Borrelia burgdorferi infections and studies on taxonomic classification. APMIS Suppl. 2002;(105):1-40. [PUBMED] Lebech AM1.
52.) Advances in Serodiagnostic Testing for Lyme Disease Are at Hand. John A Branda Barbara A Body Jeff Boyle Bernard M Branson Raymond J Dattwyler Erol Fikrig Noel J Gerald Maria Gomes-Solecki Martin Kintrup Michel Ledizet ... Show more
Clinical Infectious Diseases, cix943, https://doi.org/10.1093/cid/cix943
53.) IGENEX.com
https://www.igenex.com/testing/diagnostic-tests-for-borrelliosis/
54.) Zoonotic Leprosy in the Southeastern United States. Emerg Infect Dis. 2015 Dec;21(12):2127-34. doi: 10.3201/eid2112.150501. [PUBMED] Sharma R, Singh P, Loughry WJ, Lockhart JM, Inman WB, Duthie MS, Pena MT, Marcos LA, Scollard DM, Cole ST, Truman RW.
55) Red squirrels in the British Isles are infected with leprosy bacilli. Science. 2016 Nov 11;354(6313):744-747. [PUBMED] Avanzi C1, Del-Pozo J2, Benjak A1, Stevenson K3, Simpson VR4, Busso P1, McLuckie J3, Loiseau C1, Lawton C5, Schoening J6, Shaw DJ2, Piton J1, Vera-Cabrera L7, Velarde-Felix JS7, McDermott F6, Gordon SV6,8,9,10, Cole ST11, Meredith AL12.
56.) Why are there several species of Borrelia burgdorferi sensu lato detected in dogs and humans?. Infect Genet Evol. 2014 Apr;23:182-8. doi: 10.1016/j.meegid.2014.02.014. Epub 2014 Mar 5. [PUBMED] Skotarczak B1.
57.) Tick-borne pathogens in ticks collected from birds in Taiwan. Parasit Vectors. 2017 Nov 25;10(1):587. doi: 10.1186/s13071-017-2535-4. [PUBMED]. Kuo CC1, Lin YF2, Yao CT3, Shih HC4, Chung LH4, Liao HC4, Hsu YC5, Wang HC6
58.) Prevalence of ticks and tick-borne pathogens: Babesia and Borrelia species in ticks infesting cats of Great Britain.. Vet Parasitol. 2017 Sep 15;244:129-135. doi: 10.1016/j.vetpar.2017.07.033. Epub 2017 Aug 1. [PUBMED] Davies S1, Abdullah S2, Helps C3, Tasker S3, Newbury H4, Wall R2.
59.) Vaccination of horses with Lyme vaccines for dogs induces short-lasting antibody responses.Vaccine. 2017 Jul 24;35(33):4140-4147. doi: 10.1016/j.vaccine.2017.06.052. Epub 2017 Jun 28. [PUBMED] Guarino C1, Asbie S1, Rohde J1, Glaser A1, Wagner B2.
60.) Evaluation of 16S rRNA qPCR for detection of Mycobacterium leprae DNA in nasal secretion and skin biopsy samples from multibacillary and paucibacillary leprosy cases.Pathog Glob Health. 2017 Dec 26:1-7. doi: 10.1080/20477724.2017.1415736. [Epub ahead of print] [PUBMED] Marques LÉC1, Frota CC1, Quetz JDS2, Bindá AH2, Mota RMS3, Pontes MAA4, Gonçalves HS4, Kendall C5, Kerr LRFS6.
61.) Evidence of In Vivo Existence of Borrelia Biofilm in Borrelial Lymphocytomas. Eur J Microbiol Immunol (Bp). 2016 Feb 9;6(1):9-24. doi: 10.1556/1886.2015.00049. eCollection 2016. [PUBMED]. Sapi E1, Balasubramanian K1, Poruri A1, Maghsoudlou JS1, Socarras KM1, Timmaraju AV1, Filush KR1, Gupta K1, Shaikh S1, Theophilus PA1, Luecke DF1, MacDonald A1, Zelger B2.
62.) Molecular detection of multi drug resistant Mycobacterium leprae from Indian leprosy patients.
J Glob Antimicrob Resist. 2017 Oct 30. pii: S2213-7165(17)30197-2. doi: 10.1016/j.jgar.2017.10.010. [Epub ahead of print] [PUBMED] Lavania M1, Singh I2, Turankar RP2, Ahuja M2, Pathak V2, Sengupta U2, Das L3, Kumar A4, Darlong J5, Nathan R6, Maseey A7.
63.) Activity of Sulfa Drugs and Their Combinations against Stationary Phase B. burgdorferi In Vitro. Antibiotics (Basel). 2017 Mar 22;6(1). pii: E10. doi: 10.3390/antibiotics6010010. [PUBMED]
Feng J1, Zhang S2, Shi W3, Zhang Y4.
64.) Identification of Additional Anti-Persister Activity against Borrelia burgdorferi from an FDA Drug Library. Antibiotics (Basel). 2015 Sep 16;4(3):397-410. doi: 10.3390/antibiotics4030397. [PUBMED] Feng J1, Weitner M2, Shi W3, Zhang S4, Sullivan D5, Zhang Y6.
65.) THE WHO Antimicrobial resistance. Updated November 2017
http://www.who.int/mediacentre/factsheets/fs194/en/
66.) van Rensburg CE, Gatner EM, Imkamp FM, Anderson R (May 1982). "Effects of clofazimine alone or combined with dapsone on neutrophil and lymphocyte functions in normal individuals and patients with lepromatous leprosy". Antimicrob. Agents Chemother. 21 (5): 693–7. doi:10.1128/aac.21.5.693. PMC 181995 Freely accessible. PMID 7049077.
67.) Rifampin". The American Society of Health-System Pharmacists. Archived from the original on 2015-09-07. Retrieved Aug 1, 2015.
68.) Leschine, S.B.; Canale-Parola, E. (December 1980). "Rifampin as a Selective Agent for the Isolation of Oral Spirochetes" (PDF). Journal of Clinical Microbiology. 12 (6): 792–795. PMC 273700 Freely accessible. PMID 7309842. Archived (PDF) from the original on 8 September 2017. Retrieved 3 March 2016.
69.) A Non-human Primate Model for Rectally Transmitted Syphilis. J Infect Dis. 2017 Dec 22. doi: 10.1093/infdis/jix669. [Epub ahead of print] [PUBMED].Tansey C1, Zhao C2, Hopkins A3, Ritter JM4, Fakile YF3, Pillay A3, Katz SS3, Pereira L3, Mitchell J4, Deyounks F2, Kersh EN3, McNicholl JM4, Vishwanathan SA5.
70.) Possible cases of leprosy from the Late Copper Age (3780-3650 cal BC) in Hungary. PLoS One. 2017 Oct 12;12(10):e0185966. doi: 10.1371/journal.pone.0185966. eCollection 2017. [PUBMED] Köhler K1, Marcsik A2, Zádori P3, Biro G3, Szeniczey T4, Fábián S5, Serlegi G1, Marton T1, Donoghue HD6, Hajdu T
========================================================================
REFERENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
=====================================================================
1.) Activity of Sulfa Drugs and Their Combinations against Stationary Phase B. burgdorferi In Vitro. Antibiotics (Basel). 2017 Mar 22;6(1). pii: E10. doi: 10.3390/antibiotics6010010. [PUBMED]
Feng J1, Zhang S2, Shi W3, Zhang Y4.
2.) The Use of Dapsone as a Novel “Persister” Drug in the Treatment of Chronic
Lyme Disease/Post Treatment Lyme Disease Syndrome. Richard I Horowitz, MD and Phyllis Freeman, PhD. Hudson Valley Healing Arts Center, New York, USA
3.) Identification of novel activity against Borrelia burgdorferi persisters using an FDA approved drug library. Emerg Microbes Infect. 2014 Jul;3(7):e49. doi: 10.1038/emi.2014.53. Epub 2014 Jul 2. [PUBMED] Feng J1, Wang T1, Shi W1, Zhang S1, Sullivan D1, Auwaerter PG2, Zhang Y1.
4.) A Drug Combination Screen Identifies Drugs Active against Amoxicillin-Induced Round Bodies of In Vitro Borrelia burgdorferi Persisters from an FDA Drug Library. Front Microbiol. 2016 May 23;7:743. doi: 10.3389/fmicb.2016.00743. eCollection 2016. [PUBMED] Feng J1, Shi W1, Zhang S1, Sullivan D1, Auwaerter PG2, Zhang Y1.
5.) In vitro susceptibility of Borrelia burgdorferi isolates to three antibiotics commonly used for treating equine Lyme disease. BMC Vet Res. 2017 Sep 29;13(1):293. doi: 10.1186/s12917-017-1212-3. [PUBMED] Caol S1,2, Divers T3, Crisman M4, Chang YF1.
6.) Enfermedad de Lyme crónica y coinfecciones : diagnóstico diferencial. Open Neurol J. 2012; 6: 158-78. doi: 10.2174 / 1874205X01206010158. Epub 2012 28 de diciembre. [PUBMED]Berghoff W 1 .
7.) In vitro and in vivo antibiotic susceptibility of Lyme disease Borrelia isolated from the ixodid tick in Japan. J Dermatol. 1995 Dec;22(12):935-8. [PUBMED] Fujita H1, Yamada K, Kurita T, Masuzawa T, Yanagihara Y.
8.) Minocycline in lepromatous leprosy. Int J Lepr Other Mycobact Dis, 63(1):8-17 1995 Mar
[PUBMED] Fajardo TT Jr; Villahermosa LG; dela Cruz EC; Abalos RM; Franzblau SG; Walsh GP
9.) Efficacy of minocycline in single dose and at 100 mg twice daily for lepromatous leprosy. Int J Lepr Other Mycobact Dis (United States), Dec 1994, 62(4) p568-73 . Gelber RH; Murray LP; Siu P; Tsang M; Rea AUTHOR'S ADDRESS: San Francisco Regional Hansen's Disease Program, CA 94115.
10.) Field trial on efficacy of supervised monthly dose of 600 mg rifampin, 400 mg ofloxacin and 100 mg minocycline for the treatment of leprosy; first results. Int J Lepr Other Mycobact Dis, 65(2):224-9 1997 Jun. Mane I; Cartel JL; Grosset JH
11.) Bactericidal activity of a single-dose combination of ofloxacin plus minocycline, with or without rifampin, against Mycobacterium leprae in mice and in lepromatous patients. Antimicrob Agents Chemother, 42(5):1115-20 1998 May. [PUBMED] Ji B; Sow S; Perani E; Lienhardt C; Diderot V; Grosset J
12.)Efficacy of single dose multidrug therapy for the treatment of single-lesion paucibacillary leprosy. Single-lesion Multicentre Trial Group. Indian J Lepr, 69(2):121-9 1997 Apr-Jun [PUBMED] no author listed.
13.) Bactericidal activity of single dose of clarithromycin plus minocycline, with or without ofloxacin, against Mycobacterium leprae in patients. Antimicrob Agents Chemother, 40(9):2137-41 1996 Sep [PUBMED] Ji B; Jamet P; Perani EG; Sow S; Lienhardt C; Petinon C; Grosset JH
14.) Chronic Lyme borreliosis at the root of multiple sclerosis--is a cure with antibiotics attainable? Med Hypotheses. 2005;64(3):438-48. [PUBMED] Fritzsche M1.
15.) Hansen's Disease and Rheumatoid Arthritis Crossover of Clinical Symptoms: A Case Series of 18 Patients in the United States. Am J Trop Med Hyg. 2017 Dec;97(6):1726-1730. doi: 10.4269/ajtmh.17-0197. Epub 2017 Oct 19. [PUBMED] Labuda SM1, Schieffelin JS1, Shaffer JG2, Stryjewska BM3.
16.) Leprosy - an overview of clinical features, diagnosis, and treatment. J Dtsch Dermatol Ges. 2017 Aug;15(8):801-827. doi: 10.1111/ddg.13301. [PUBMED] Fischer M1.
17.) Multidrug therapy for leprosy: a game changer on the path to elimination. Lancet Infect Dis. 2017 Sep;17(9):e293-e297. doi: 10.1016/S1473-3099(17)30418-8. Epub 2017 Jul 7. [PUBMED]Smith CS1, Aerts A2, Saunderson P3, Kawuma J4, Kita E5, Virmond M6.
18.) Infectious neuropathies. Neurol Clin. 2007 Feb;25(1):115-37. [PUBMED] Said G1.
19.) A case presentation of bilateral simultaneous Bell's palsy. Am J Otolaryngol. 2003 Jul-Aug;24(4):271-3. [PUBMED] Kilic R1, Ozdek A, Felek S, Safak MA, Samim E.
20.) Inflammatory neuropathies associated with known infections (HIV, leprosy, Chagas' disease, Lyme disease). Baillieres Clin Neurol. 1994 Apr;3(1):149-71. [PUBMED] Said G1.
21.) Antibiotic-refractory Lyme arthritis is associated with HLA-DR molecules that bind a Borrelia
burgdorferi peptide. J Exp Med. 2006 Apr 17;203(4):961-71. Epub 2006 Apr 3. [PUBMED] Steere AC1, Klitz W, Drouin EE, Falk BA, Kwok WW, Nepom GT, Baxter-Lowe LA.
22.) HLA-DR alleles determine responsiveness to Borrelia burgdorferi antigens in a mouse model of self-perpetuating arthritis. Arthritis Rheum. 2009 Dec;60(12):3831-40. doi: 10.1002/art.25005.
[PUBMED] Iliopoulou BP1, Guerau-de-Arellano M, Huber BT.
23.) Association of treatment-resistant chronic Lyme arthritis with HLA-DR4 and antibody reactivity to OspA and OspB of Borrelia burgdorferi. Infect Immun. 1993 Jul;61(7):2774-9. [PUBMED] Kalish RA1, Leong JM, Steere AC.
24.) HLA-B*13:01 and the dapsone hypersensitivity syndrome. N Engl J Med. 2013 Oct 24;369(17):1620-8. doi: 10.1056/NEJMoa1213096. [PUBMED] Zhang FR1, Liu H, Irwanto A, Fu XA, Li Y, Yu GQ, Yu YX, Chen MF, Low HQ, Li JH, Bao FF, Foo JN, Bei JX, Jia XM, Liu J, Liany H, Wang N, Niu GY, Wang ZZ, Shi BQ, Tian HQ, Liu HX, Ma SS, Zhou Y, You JB, Yang Q, Wang C, Chu TS, Liu DC, Yu XL, Sun YH, Ning Y, Wei ZH, Chen SL, Chen XC, Zhang ZX, Liu YX, Pulit SL, Wu WB, Zheng ZY, Yang RD, Long H, Liu ZS, Wang JQ, Li M, Zhang LH, Wang H, Wang LM, Xiao P, Li JL, Huang ZM, Huang JX, Li Z, Liu J, Xiong L, Yang J, Wang XD, Yu DB, Lu XM, Zhou GZ, Yan LB, Shen JP, Zhang GC, Zeng YX, de Bakker PI, Chen SM, Liu JJ.
25.) Increase in the incidence of dapsone hypersensitivity syndrome--an appraisal. Lepr Rev. 2001 Mar;72(1):57-62. [PUBMED] Rao PN1, Lakshmi TS.
26.) Associations of HLA DR and DQ molecules with Lyme borreliosis in Latvian patients. BMC Res Notes. 2012 Aug 14;5:438. doi: 10.1186/1756-0500-5-438. [PUBMED] Kovalchuka L1, Eglite J, Lucenko I, Zalite M, Viksna L, Krumiņa A.
27.) Minocycline hepatotoxicity: Clinical characterization and identification of HLA-B∗35:02 as a risk factor. J Hepatol. 2017 Jul;67(1):137-144. doi: 10.1016/j.jhep.2017.03.010. Epub 2017 Mar 18. [PUBMED] Urban TJ1, Nicoletti P2, Chalasani N3, Serrano J4, Stolz A5, Daly AK6, Aithal GP7, Dillon J8, Navarro V9, Odin J10, Barnhart H11, Ostrov D12, Long N1, Cirulli ET11, Watkins PB1, Fontana RJ13; Drug-Induced Liver Injury Network (DILIN); Pharmacogenetics of Drug-Induced Liver Injury group (DILIGEN); International Serious Adverse Events Consortium (iSAEC).
28.) Advances in Serodiagnostic Testing for Lyme Disease Are at Hand. Clin Infect Dis. 2017 Dec 7. doi: 10.1093/cid/cix943. [Epub ahead of print] [PUBMED] Branda JA1, Body BA2, Boyle J3, Branson BM4, Dattwyler RJ5, Fikrig E6, Gerald NJ7, Gomes-Solecki M8, Kintrup M9, Ledizet M10, Levin AE11, Lewinski M12, Liotta LA13, Marques A14, Mead PS15, Mongodin EF16, Pillai S17, Rao P7, Robinson WH18, Roth KM7, Schriefer ME15, Slezak T19, Snyder J20, Steere AC21, Witkowski J22, Wong SJ23, Schutzer SE24.
29.) Hall, Stephen S (November 2011). "Iceman Autopsy". National Geographic. Archived from the original on 19 October 2011. Retrieved 17 October 2011.
30.) Josselyn, John (1670). An Account of Two Voyages to New-England Made during the Years 1638, 1663. Archived from the original on 25 June 2013.page 92
31.) Hoen AG, Margos G, Bent SJ, et al. (September 2009). "Phylogeography of Borrelia burgdorferi in the eastern United States reflects multiple independent Lyme disease emergence events". Proc. Natl. Acad. Sci. U.S.A. 106 (35): 15013–18. Bibcode:2009PNAS..10615013H. doi:10.1073/pnas.0903810106. JSTOR 40484546. PMC 2727481 Freely accessible. PMID 19706476. Lay summary – YaleNews (10 August 2009).
32.) Drymon, MM (2008). Disguised as the devil: how Lyme disease created witches and changed history. pp. 51–52. ISBN 978-0-615-20061-3.
33.) Summerton N (1995). "Lyme disease in the eighteenth century". BMJ. 311 (7018): 1478. doi:10.1136/bmj.311.7018.1478.
34.) Holy bible: Genesis: 12; Exodus: 8: 6-9: 7; Leviticus, 13:12, Leviticus: 15
35.) Harper, KN; Zuckerman, MK; Harper, ML; Kingston, JD; Armelagos, GJ (2011). "The origin and antiquity of syphilis revisited: an appraisal of Old World pre-Columbian evidence for treponemal infection". American Journal of Physical Anthropology. 146 Suppl 53: 99–133. doi:10.1002/ajpa.21613. PMID 22101689.
36.) Winters, Adam (2006). Syphilis. New York: Rosen Pub. Group. p. 17. ISBN 9781404209060. Archived from the original on 4 March 2016.
37.) Dormandy, Thomas (2006). The worst of evils: man's fight against pain: a history (Uncorrected page proof. ed.). New Haven: Yale University Press. p. 99. ISBN 978-0300113228.
38.) Anthony Grafton (March 1995). "Drugs and Diseases: New World Biology and Old World Learning". New Worlds, Ancient Texts The Power of Tradition and the Shock of Discovery. Harvard University Press. pp. 159–194. ISBN 9780674618763.
39.) Identification of the leprosy agent Mycobacterium lepromatosis in Singapore.
J Drugs Dermatol. 2012 Feb;11(2):168-72. [PUBMED] Han XY1, Sizer KC, Tan HH.
40.) Mutations in the drug resistance-determining region of Mycobacterium lepromatosis isolated from leprosy patients in Mexico. J Dermatol. 2016 Nov;43(11):1345-1349. doi: 10.1111/1346-8138.13483. Epub 2016 Jun 27. [PUBMED] Kai M1, Fafutis-Morris M2, Miyamoto Y3, Mukai T3, Mayorga-Rodriguez J2, Rodriguez-Castellanos MA2, Martínez-Guzman MA2, Matsuoka M3.
41.) Farhi, D; Dupin, N (Sep–Oct 2010). "Origins of syphilis and management in the immunocompetent patient: facts and controversies". Clinics in dermatology. 28 (5): 533–8. doi:10.1016/j.clindermatol.2010.03.011. PMID 20797514.
42.) Franzen, C (December 2008). "Syphilis in composers and musicians--Mozart, Beethoven, Paganini, Schubert, Schumann, Smetana". European Journal of Clinical Microbiology & Infectious Diseases. 27 (12): 1151–7. doi:10.1007/s10096-008-0571-x. PMID 18592279.
43.) Fracastor, Hieronymus (1911). Syphilis. The Philmar Company. "Syphilis". Online Etymology Dictionary. 2001.
44.) Raju T (2006). "Hot brains: manipulating body heat to save the brain" (PDF). Pediatrics. 117 (2): e320–1.
45.) Early syphilis: serological treatment response to doxycycline/tetracycline versus benzathine penicillin. J Infect Dev Ctries. 2014 Feb 13;8(2):228-32. doi: 10.3855/jidc.3013. [PUBMED] . Li J1, Zheng HY.
46.) Surveillance for Borrelia burgdorferi in Ixodes Ticks and Small Rodents in British Columbia.
Vector Borne Zoonotic Dis. 2015 Nov;15(11):701-5. doi: 10.1089/vbz.2015.1854. Epub 2015 Oct 26. [PUBMED] Morshed MG1,2, Lee MK1, Man S1, Fernando K1, Wong Q1, Hojgaard A3, Tang P1,2, Mak S4, Henry B2,5, Patrick DM2,4.
47.) Borrelia miyamotoi Infections in Humans and Ticks, Northeastern China. Emerg Infect Dis. 2018 Feb;24(2):236-241. doi: 10.3201/eid2402.160378. [PUBMED] Jiang BG, Jia N, Jiang JF, Zheng YC, Chu YL, Jiang RR, Wang YW, Liu HB, Wei R, Zhang WH, Li Y, Xu XW, Ye JL, Yao NN, Liu XJ, Huo QB, Sun Y, Song JL, Liu W, Cao WC.
48.) A simple method for the detection of live Borrelia spirochaetes in human blood using classical microscopy techniques. Morten Motzfeldt Laane, Ivar Mysterud. Published 2013. Semantic Sholar. Source: https://www.semanticscholar.org/paper/A-simple-method-for-the-detection-of-live-Borrelia-Laane-Mysterud/4f6251e40f196b094905d84e87b8b6fe8d1d1636
49.) Pustular secondary syphilis: report of three cases and review of the literature. Int J Dermatol. 2014 Oct;53(10):e428-31. doi: 10.1111/ijd.12337. Epub 2014 Sep 10. [PUBMED]Kazlouskaya V1, Wittmann C, Tsikhanouskaya I.
50.) Serological Evidence of Borrelia Burgdorferi Infection in Mexican Patients with Facial Palsy. Rev Invest Clin. 2017 Nov-Dec;69(6):344-348. doi: 10.24875/RIC.17002344. [PUBMED] Gordillo-Pérez G1, García-Juárez I1, Solórzano-Santos F2, Corrales-Zúñiga L3, Muñoz-Hernández O2, Torres-López J1.
51.) Polymerase chain reaction in diagnosis of Borrelia burgdorferi infections and studies on taxonomic classification. APMIS Suppl. 2002;(105):1-40. [PUBMED] Lebech AM1.
52.) Advances in Serodiagnostic Testing for Lyme Disease Are at Hand. John A Branda Barbara A Body Jeff Boyle Bernard M Branson Raymond J Dattwyler Erol Fikrig Noel J Gerald Maria Gomes-Solecki Martin Kintrup Michel Ledizet ... Show more
Clinical Infectious Diseases, cix943, https://doi.org/10.1093/cid/cix943
53.) IGENEX.com
https://www.igenex.com/testing/diagnostic-tests-for-borrelliosis/
54.) Zoonotic Leprosy in the Southeastern United States. Emerg Infect Dis. 2015 Dec;21(12):2127-34. doi: 10.3201/eid2112.150501. [PUBMED] Sharma R, Singh P, Loughry WJ, Lockhart JM, Inman WB, Duthie MS, Pena MT, Marcos LA, Scollard DM, Cole ST, Truman RW.
55) Red squirrels in the British Isles are infected with leprosy bacilli. Science. 2016 Nov 11;354(6313):744-747. [PUBMED] Avanzi C1, Del-Pozo J2, Benjak A1, Stevenson K3, Simpson VR4, Busso P1, McLuckie J3, Loiseau C1, Lawton C5, Schoening J6, Shaw DJ2, Piton J1, Vera-Cabrera L7, Velarde-Felix JS7, McDermott F6, Gordon SV6,8,9,10, Cole ST11, Meredith AL12.
56.) Why are there several species of Borrelia burgdorferi sensu lato detected in dogs and humans?. Infect Genet Evol. 2014 Apr;23:182-8. doi: 10.1016/j.meegid.2014.02.014. Epub 2014 Mar 5. [PUBMED] Skotarczak B1.
57.) Tick-borne pathogens in ticks collected from birds in Taiwan. Parasit Vectors. 2017 Nov 25;10(1):587. doi: 10.1186/s13071-017-2535-4. [PUBMED]. Kuo CC1, Lin YF2, Yao CT3, Shih HC4, Chung LH4, Liao HC4, Hsu YC5, Wang HC6
58.) Prevalence of ticks and tick-borne pathogens: Babesia and Borrelia species in ticks infesting cats of Great Britain.. Vet Parasitol. 2017 Sep 15;244:129-135. doi: 10.1016/j.vetpar.2017.07.033. Epub 2017 Aug 1. [PUBMED] Davies S1, Abdullah S2, Helps C3, Tasker S3, Newbury H4, Wall R2.
59.) Vaccination of horses with Lyme vaccines for dogs induces short-lasting antibody responses.Vaccine. 2017 Jul 24;35(33):4140-4147. doi: 10.1016/j.vaccine.2017.06.052. Epub 2017 Jun 28. [PUBMED] Guarino C1, Asbie S1, Rohde J1, Glaser A1, Wagner B2.
60.) Evaluation of 16S rRNA qPCR for detection of Mycobacterium leprae DNA in nasal secretion and skin biopsy samples from multibacillary and paucibacillary leprosy cases.Pathog Glob Health. 2017 Dec 26:1-7. doi: 10.1080/20477724.2017.1415736. [Epub ahead of print] [PUBMED] Marques LÉC1, Frota CC1, Quetz JDS2, Bindá AH2, Mota RMS3, Pontes MAA4, Gonçalves HS4, Kendall C5, Kerr LRFS6.
61.) Evidence of In Vivo Existence of Borrelia Biofilm in Borrelial Lymphocytomas. Eur J Microbiol Immunol (Bp). 2016 Feb 9;6(1):9-24. doi: 10.1556/1886.2015.00049. eCollection 2016. [PUBMED]. Sapi E1, Balasubramanian K1, Poruri A1, Maghsoudlou JS1, Socarras KM1, Timmaraju AV1, Filush KR1, Gupta K1, Shaikh S1, Theophilus PA1, Luecke DF1, MacDonald A1, Zelger B2.
62.) Molecular detection of multi drug resistant Mycobacterium leprae from Indian leprosy patients.
J Glob Antimicrob Resist. 2017 Oct 30. pii: S2213-7165(17)30197-2. doi: 10.1016/j.jgar.2017.10.010. [Epub ahead of print] [PUBMED] Lavania M1, Singh I2, Turankar RP2, Ahuja M2, Pathak V2, Sengupta U2, Das L3, Kumar A4, Darlong J5, Nathan R6, Maseey A7.
63.) Activity of Sulfa Drugs and Their Combinations against Stationary Phase B. burgdorferi In Vitro. Antibiotics (Basel). 2017 Mar 22;6(1). pii: E10. doi: 10.3390/antibiotics6010010. [PUBMED]
Feng J1, Zhang S2, Shi W3, Zhang Y4.
64.) Identification of Additional Anti-Persister Activity against Borrelia burgdorferi from an FDA Drug Library. Antibiotics (Basel). 2015 Sep 16;4(3):397-410. doi: 10.3390/antibiotics4030397. [PUBMED] Feng J1, Weitner M2, Shi W3, Zhang S4, Sullivan D5, Zhang Y6.
65.) THE WHO Antimicrobial resistance. Updated November 2017
http://www.who.int/mediacentre/factsheets/fs194/en/
66.) van Rensburg CE, Gatner EM, Imkamp FM, Anderson R (May 1982). "Effects of clofazimine alone or combined with dapsone on neutrophil and lymphocyte functions in normal individuals and patients with lepromatous leprosy". Antimicrob. Agents Chemother. 21 (5): 693–7. doi:10.1128/aac.21.5.693. PMC 181995 Freely accessible. PMID 7049077.
67.) Rifampin". The American Society of Health-System Pharmacists. Archived from the original on 2015-09-07. Retrieved Aug 1, 2015.
68.) Leschine, S.B.; Canale-Parola, E. (December 1980). "Rifampin as a Selective Agent for the Isolation of Oral Spirochetes" (PDF). Journal of Clinical Microbiology. 12 (6): 792–795. PMC 273700 Freely accessible. PMID 7309842. Archived (PDF) from the original on 8 September 2017. Retrieved 3 March 2016.
69.) A Non-human Primate Model for Rectally Transmitted Syphilis. J Infect Dis. 2017 Dec 22. doi: 10.1093/infdis/jix669. [Epub ahead of print] [PUBMED].Tansey C1, Zhao C2, Hopkins A3, Ritter JM4, Fakile YF3, Pillay A3, Katz SS3, Pereira L3, Mitchell J4, Deyounks F2, Kersh EN3, McNicholl JM4, Vishwanathan SA5.
70.) Possible cases of leprosy from the Late Copper Age (3780-3650 cal BC) in Hungary. PLoS One. 2017 Oct 12;12(10):e0185966. doi: 10.1371/journal.pone.0185966. eCollection 2017. [PUBMED] Köhler K1, Marcsik A2, Zádori P3, Biro G3, Szeniczey T4, Fábián S5, Serlegi G1, Marton T1, Donoghue HD6, Hajdu T
71.) Lapenta, P. Conversatorio sobre Lepra y su
diagnostico (1984-1987) Consultorio Para Enfermedades de la Piel,. Maracay
Estado Aragua Venezuela.
Producido Por Dr. José Lapenta R. Dermatólogo
Maracay Estado Aragua Venezuela 2.017-2.023
Telf: 04142976087- 04127766810
04166401045
Follow @dermagicexpress



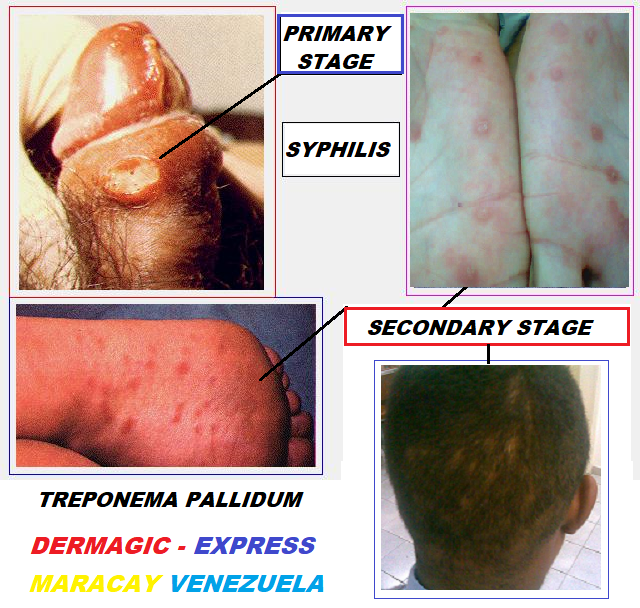
No hay comentarios:
Publicar un comentario
Tu comentario será objeto de revisión y luego aprobado.
Your comment will be revised and then approved.