El síndrome de Larva Migrans Cutáneo y las mascotas (perros y gatos). !!!
The Cutaneous Larva Migrans Syndrome and pets (dogs and cats).
!!!
Actualizado 2025
EDITORIAL ESPAÑOL
====================
Hola amigos de la red, DERMAGIC de nuevo con ustedes. El tema de hoy EL SÍNDROME LARVA MIGRANS CUTÁNEA, Y LAS MASCOTAS (PERROS Y GATOS)
====================
Hola amigos de la red, DERMAGIC de nuevo con ustedes. El tema de hoy EL SÍNDROME LARVA MIGRANS CUTÁNEA, Y LAS MASCOTAS (PERROS Y GATOS)
Nos encantan las mascotas, sobre todo los perros y gatos. Pero en
la mierda (caca) de estos bellos
animales hay unos parásitos que pueden pasar a la piel cuando la
tocamos o ingerimos,
El sitio favorito para contraerla es la
PLAYA o el CAMPO donde nuestras lindas mascotas hacen
su mierda. Luego venimos nosotros e ingenuamente ponemos en
contacto alguna parte de nuestro cuerpo (principalmente el pie) con el pupú-caca,
y la larva penetra nuestra piel directamente desde las heces provocando
la enfermedad.
También en los hogares donde hay perros y gatos no controlados
por el veterinario. En fin una enfermedad más donde el hombre
es accidentalmente contaminado por el animal.
Hoy en dia descrita en algunas publicaciones como "el souvenir de los viajeros y turistas" que la contraen en sus
viajes de vacaciones. Varios parásitos son los agentes causales pero
los más comunes son: ANCYLOSTOMA CANInum y ANQUILOSTOMA. BRAZILIENSE.
OTROS AGENTES CAUSALES:
- Ancylostoma ceylanicum, A. tubaeforme (perros y gatos)
- Gnathostoma spinigerum (gatos, perros, cerdos)
- Gnathostoma spinigerum (gatos, perros, cerdos)
- Uncinaria stenocephala (perros en Europa)
- Bunostomum phlebotomum (ganado)
- Pelodera strongyloides
- En raros casos, Ancylostoma duodenale, Necator americanus (uncinarias humanas), y strongyloides stercoralis.
- Bunostomum phlebotomum (ganado)
- Pelodera strongyloides
- En raros casos, Ancylostoma duodenale, Necator americanus (uncinarias humanas), y strongyloides stercoralis.
La LARVA MIGRANS CUTÁNEA, es una enfermedad SUPERFICIAL, el parásito vive en la capa superficial de la piel, haciendo
túneles a medida que crece, denominada también "erupción progresiva o
serpigimosa", pero es auto limitada y con un buen tratamiento desaparece
sin dejar complicaciones en la mayoría de los casos.
La LARVA MIGRANS CUTÁNEA presenta una variante denominada
PANICULITIS NODULAR MIGRATORIA: se presenta cuando las larvas migran hacia el panículo adiposo
(mas profundamente), formando nódulos, subcutáneos migratorios, edema y
eosinofilia. Los agentes causales que producen esta variante son:
- Gnathostoma spinigerum.
- Gnathostoma doloresis.
- Gnathostoma hispidum.
LARVA MIGRANS VISCERAL:
Hay otra variante de la LARVA MIGRANS QUE ES
LA VISCERAL (PROFUNDA)
causada por otros parásitos como el Toxocara canis (Perro) y otros
mas, donde el el parásito "migra: a órganos profundos como:
CAVIDAD VISCERAL OJO, CEREBRO, MÚSCULOS Y OTROS. esta es más peligrosa y puede dejar secuelas si no es detectada y
tratada a tiempo.
AGENTES CAUSANTES DE LARVA MIGRANS VISCERAL:
- Toxocara canis (perros)
- Toxocara cati (gatos)
TRATAMIENTOS DE LA LARVA MIGRANS:
1.) Ivermectina:
Dosis: 200 mcg/kg (0.2 mg/kg) en dosis única (puede repetirse a los 7-14 días si persisten lesiones), para un adulto de 60 kg le corresponderían 2 pastillas de 6 mgr de ivermectin, que es la presentación original. Considerado actualmente el tratamiento mas eficaz.
Dosis: 200 mcg/kg (0.2 mg/kg) en dosis única (puede repetirse a los 7-14 días si persisten lesiones), para un adulto de 60 kg le corresponderían 2 pastillas de 6 mgr de ivermectin, que es la presentación original. Considerado actualmente el tratamiento mas eficaz.
2.) Albendazol:
La dosis es de 400 mgr dia por 3 a 4 dias seguidos. Se recomienda
repetir a la semana 3 o 4 dias mas. Tratamiento muy útil en los
niños, pues la presentación es también en suspension, aparte de las
tabletas que son de 200 mgr.
3.) Tiabendazol: (drofen):
3.) Tiabendazol: (drofen):
Dosis 25 mg/kg dia, por 2-5 dias (promedio 3 dias). No disponible en
Venezuela hoy dia.
TRATAMIENTO LOCAL:
- Criocirugia: (casi en
desuso por ser muy dolorosa), consiste aplicar "nitrógeno liquido" desde
afuera en el trayecto de la lesion, la larva muere por
"enfriamiento".
- Formulas magistrales: que
contienen albendazol o tinidazol para ser aplicadas externamente: la
absorción percutanea de las misma, "envenena" el parásito y
muere.
TRATAMIENTO SINTOMÁTICO:
- Antibióticos: si hay infección secundaria.
- Antihistamínicos orales:
Para controlar el prurito que puede ser intenso.
- Corticoides topicos: Para
disminuir la inflamación y evitar infección secundaria.
El tratamiento de la
LARVA MIGRANS PROFUNDA VISCERAL y OCULAR., suele ser mas prolongado, 6 a 18 meses promedio. El tratamiento de
la LARVA ocular puede incluir cirugía vitroretiniana, fotocoagulación
por láser y medicación para evitar daño ocular.
CONCLUSIONES:
- Instaurar tratamiento temprano para evitar secuelas organicas,
principalmente en los casos VISCERALES y OCULARES.
- La LARVA MIGRANS CUTANEA, clásica es relativamente fácil de
identificar y los tratamientos propuestos son altamente
efectivos.
- De modo pues que cuiden las lindas mascotas, llévenlas regularmente al veterinario y tengan cuidado cuando vayan a la playa y el campo para evitar esta enfermedad.
- De modo pues que cuiden las lindas mascotas, llévenlas regularmente al veterinario y tengan cuidado cuando vayan a la playa y el campo para evitar esta enfermedad.
En las referencias conocerás la enfermedad y sus variantes, los
agentes causales y las opciones terapéuticas
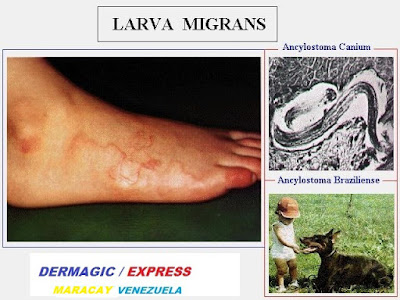
En el attach: la larva, el niño, la mascota, y otras más.
En el attach: la larva, el niño, la mascota, y otras más.
Dr. José M. Lapenta
EDITORIAL ENGLISH
===================
Hello friends of to the net, DERMAGIC again with you. Today's topic THE CUTANEOUS LARVA MIGRANS SYNDROME AND PETS (DOGS AND CATS).
===================
Hello friends of to the net, DERMAGIC again with you. Today's topic THE CUTANEOUS LARVA MIGRANS SYNDROME AND PETS (DOGS AND CATS).
We love pets, mainly the dogs and cats. But in the feces (poop)
of these beautiful animals there are some parasites that can pass
to the skin when we touch or ingest them.
The favorite site to contract them is the BEACH or THE FIELD
where our pretty pets make its feces. Then we come and
frankly we put some part of our body (mainly the foot) in contact
with them, and the larva penetrates our skin directly from the feces causing the
disease.
Also in homes where there are dogs and cats not controlled by the
veterinarian. In short another disease where the man is accidentally
contaminated by the animal.
Nowadays described in some publications as "the souvenir of travelers and
tourists" who contract it during their vacations. Several parasites are
the causal agents but the most common are: ANCYLOSTOMA CANNINUM and
ANCYLOSTOMA BRAZILIENZE.
OTHER CAUSING AGENTS:
- Ancylostoma ceylanicum, A. tubaeforme (dogs and cats)
- Gnathostoma spinigerum (cats, dogs, pigs)
- Hookworm (dogs in Europe)
- Bunostomum phlebotomum (cattle)
- Pelodera strongyloides
- In rare cases, Ancylostoma duodenale, Necator americanus (human hookworms), and strongyloides stercoralis.
- Ancylostoma ceylanicum, A. tubaeforme (dogs and cats)
- Gnathostoma spinigerum (cats, dogs, pigs)
- Hookworm (dogs in Europe)
- Bunostomum phlebotomum (cattle)
- Pelodera strongyloides
- In rare cases, Ancylostoma duodenale, Necator americanus (human hookworms), and strongyloides stercoralis.
The
cutaneous larva migrans, is a
superficial disease, the
parasite lives in the superficial layer of the skin, making tunnels as it
grows, also called "creeping eruption", but it is self-limited and with a
good treatment disappears without leaving complications in the majority of
cases.
CUTANEOUS LARVA MIGRANS presents a variant called
MIGRATORY NODULAR PANICULITIS:
it occurs when the larvae migrate deeper into the fat pad, forming
migratory subcutaneous nodules, edema, and eosinophilia. The causative
agents that produce this variant are:
- Gnathostoma spinigerum.
- Gnathostoma doloris.
- Gnathostoma hispidum.
VISCERAL LARVA MIGRANS:
There is another variant of LARVA MIGRANS, VISCERAL (DEEP) caused by other parasites such as Toxocara canis (dogs) and others. The parasite migrates to deep organs such as the VISCERAL CAVITY, EYES, BRAIN, MUSCLES, and others. This is more dangerous and can leave after-effects if not detected and treated promptly.
CAUSING AGENTS OF VISCERAL LARVA MIGRANS:
- Toxocara canis (dogs)
- Toxocara cati (cats)
LARVA MIGRANS TREATMENTS:
1.) Ivermectin:
Dose: 200 mcg/kg (0.2 mg/kg) as a single dose (can be repeated after 7-14 days if lesions persist). For a 60 kg adult, the dose would be: Two 6 mg ivermectin tablets, which is the original formulation. Currently considered the most effective treatment.
2.) Albendazole:
- Gnathostoma spinigerum.
- Gnathostoma doloris.
- Gnathostoma hispidum.
VISCERAL LARVA MIGRANS:
There is another variant of LARVA MIGRANS, VISCERAL (DEEP) caused by other parasites such as Toxocara canis (dogs) and others. The parasite migrates to deep organs such as the VISCERAL CAVITY, EYES, BRAIN, MUSCLES, and others. This is more dangerous and can leave after-effects if not detected and treated promptly.
CAUSING AGENTS OF VISCERAL LARVA MIGRANS:
- Toxocara canis (dogs)
- Toxocara cati (cats)
LARVA MIGRANS TREATMENTS:
1.) Ivermectin:
Dose: 200 mcg/kg (0.2 mg/kg) as a single dose (can be repeated after 7-14 days if lesions persist). For a 60 kg adult, the dose would be: Two 6 mg ivermectin tablets, which is the original formulation. Currently considered the most effective treatment.
2.) Albendazole:
The dose is 400 mg daily for 3 to 4 consecutive days. It is recommended
to repeat the treatment for 3 or 4 more days a week. This treatment is
very useful in children, as it also comes in suspension form, in addition
to the 200 mg tablets.
3.) Thiabendazole (Drofen):
3.) Thiabendazole (Drofen):
Dosage: 25 mg/kg daily, for 2-5 days (average: 3 days). Not currently
available in Venezuela.
LOCAL TREATMENT:
- Cryosurgery: (almost obsolete due to its very painful nature), consists of applying "liquid nitrogen" from the outside to the lesion. The larva dies due to "cooling."
- Magistral formulations: containing albendazole or tinidazole for external application: percutaneous absorption of the It "poisons" the parasite, and it dies.
SYMPTOMATIC TREATMENT:
- Antibiotics: if there is a secondary infection.
- Oral antihistamines: To control itching, which can be intense.
- Topical corticosteroids: To reduce inflammation and prevent secondary infection.
Treatment for deep VISCERAL and OCULAR larva migrans is usually longer, averaging 6 to 18 months. Treatment for ocular larva migrans may include vitroretinal surgery, laser photocoagulation, and medication to prevent eye damage.
CONCLUSIONS:
- Establish early treatment to avoid organic sequelae, especially in visceral and ocular cases.
- Classical cutaneous larva migrans is relatively easy to identify, and the proposed treatments are highly effective.
- So, take care of your lovely pets, take them to the vet regularly, and be careful when go to the beach and the countryside to avoid this disease.
LOCAL TREATMENT:
- Cryosurgery: (almost obsolete due to its very painful nature), consists of applying "liquid nitrogen" from the outside to the lesion. The larva dies due to "cooling."
- Magistral formulations: containing albendazole or tinidazole for external application: percutaneous absorption of the It "poisons" the parasite, and it dies.
SYMPTOMATIC TREATMENT:
- Antibiotics: if there is a secondary infection.
- Oral antihistamines: To control itching, which can be intense.
- Topical corticosteroids: To reduce inflammation and prevent secondary infection.
Treatment for deep VISCERAL and OCULAR larva migrans is usually longer, averaging 6 to 18 months. Treatment for ocular larva migrans may include vitroretinal surgery, laser photocoagulation, and medication to prevent eye damage.
CONCLUSIONS:
- Establish early treatment to avoid organic sequelae, especially in visceral and ocular cases.
- Classical cutaneous larva migrans is relatively easy to identify, and the proposed treatments are highly effective.
- So, take care of your lovely pets, take them to the vet regularly, and be careful when go to the beach and the countryside to avoid this disease.
So take care of the cute pets, take them regularly to the veterinarian and
be careful when go to the beach and the countryside or field to avoid this
disease!
In the references you will know the disease and its variants, the causal
agents and the therapeutic options
In the attach: the larva, the boy, the pett, and others.
Greetings to all.
Dr. José Lapenta
Dr. José M. Lapenta
================================================================
REFERENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
================================================================
============================================================
0.) CUTANEOUS, VISCERAL and OCULAR LARVA MIGRANS
============================================================
1.) Souvenir from the Hamptons - a case of cutaneous larva migrans of six months' duration.
2.) Effectiveness of a new therapeutic regimen with albendazole in cutaneous larva migrans.
3.) [Migrant erythema as clinical presentation of cutaneous larva migrans in Mexico City]
4.) Larva migrans within scalp sebaceous gland.
5.) Cutaneous larva migrans, sacroileitis, and optic neuritis caused by an unidentified organism acquired in Thailand.
6.) Perianal cutaneous larva migrans in a child.
7.) [Infections with Baylisascaris procyonis in humans and raccoons]
8.) Cutaneous larva migrans complicated by erythema multiforme [see comments]
9.) Cutaneous larva migrans associated with water shoe use.
10.) Cutaneous larva migrans infection in the pediatric foot. A review and two case reports.
11.) Creeping eruption of larva migrans--a case report in a beach volley athlete.
12.) Albendazole: a new therapeutic regimen in cutaneous larva migrans.
13.) A primary health care approach to an outbreak of cutaneous larva migrans.
14.) Autochthonous cutaneous larva migrans in Germany.
15.) High prevalence of Ancylostoma spp. infection in dogs, associated with endemic focus of human cutaneous larva migrans, in Tacuarembo, Uruguay.
16.) Persistent cutaneous larva migrans due to Ancylostoma species.
17.) [A case of Dirofilaria repens migration in man]
18.) [Cutaneous larva migrans, autochthonous in France. Apropos of a case]
19.) Cutaneous larva migrans in travelers: synopsis of histories, symptoms, and treatment of 98 patients.
20.) [Nematode larva migrans. On two cases of filarial infection]
21.) Larva migrans that affect the mouth.
22.) Immunological studies on human larval toxocarosis.
23.) [Larva migrans]
24.) Effect of albendazole on Ancylostoma caninum larvae migrating in the muscles of mice.
25.) [Ocular manifestations of toxocariasis]
26.) Toxocara infestations in humans: symptomatic course of toxocarosis correlates significantly with levels of IgE/anti-IgE immune complexes.
27.) [Long-term observations of ocular toxocariasis in children and youth]
28.) [A case of uveitis due to gnathostoma migration into the vitreous cavity]
29.) [The ocular form of toxocariasis]
30.) [Visceral larval migrans (Human toxocariasis) cause of hypereosinophilia and visceral granulomas in adults]
31.) Visceral larva migrans syndrome complicated by liver abscess.
32.) Visceral larva migrans and tropical pyomyositis: a case report.
33.) [2 cases of toxocariasis (visceral larva migrans)]
34.) [Visceral larva migrans. A rare cause of eosinophilia in adults]
35.) [Visceral larva migrans: a mixed form of presentation in an adult. The clinical and laboratory aspects]
36.) Visceral larva migrans induced eosinophilic cardiac pseudotumor: a cause of sudden death in a child.
37.) [Toxocariasis. A cosmopolitan parasitic zoonosis]
38.) Visceral larva migrans mimicking rheumatic diseases.
39.) Hepatic granulomas due to visceral larva migrans in adults: appearance on US and MRI.
40.) [Ascaridiasis zoonoses: visceral larva migrans syndromes]
41.) Hepatic visceral larva migrans: evolution of the lesion, diagnosis, and role of high-dose albendazole therapy.
42.) Neuroimaging studies of cerebral "visceral larva migrans" syndrome. 43.)[Acute eosinophilic pneumonia and the larva migrans syndrome: apropos of a case in an adult]
44.)Toxocariasis simulating hepatic recurrence in a patient with Wilms' tumor.
45.) Hepatic imaging studies on patients with visceral larva migrans due to probable Ascaris suum infection.
46.) Encephalopathy caused by visceral larva migrans due to Ascaris suum.
47.) [Imported skin diseases (see comments)]
48.) [Incidence of Toxocara ova--especially ova of visceral larva migrans
in beach sand of Warnemunde in 1997]
49.) Pets and Parasites.
50.) Cutaneous larva migrans in travelers: synopsis of histories, symptoms, and treatment of 98 patients.
51.) Cutaneous larva migrans.
52.)[Current therapeutic possibilities in cutaneous larva migrans]
53.) Cutaneous larva migrans due to Pelodera strongyloides.
54.) Oral albendazole for the treatment of cutaneous larva migrans.
55.) Cutaneous larva migrans in northern climates. A souvenir of your dream vacation.
56.) Creeping eruption. A review of clinical presentation and management of
60 cases presenting to a tropical disease unit.
57.) Dermatoses associated with travel to tropical countries: a prospective study of the diagnosis and management of 269 patients presenting to a tropical disease unit.
58.) Larva currens and systemic disease.
59.) Hookworm folliculitis.
60.) [Prurigo and further diagnostically significant skin symptoms in strongyloidosis]
61.) Gnathostomiasis, or larva migrans profundus.
62.) Visceral larva migrans caused by Trichuris vulpis.
63.) Creeping disease due to larva of spiruroid nematoda.
64.) Creeping eruption due to larvae of the suborder Spirurina--a newly
recognized causative parasite.
65.) Linear lichen planus mimicking creeping eruption.
66.) Diagnosis and management of Baylisascaris procyonis infection in an infant with nonfatal meningoencephalitis.
67.) [Human gnathostomiasis. The first evidence of the parasite in South America]
68.) Efficacy of ivermectin in the therapy of cutaneous larva migrans
[letter]
REFERENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
================================================================
============================================================
0.) CUTANEOUS, VISCERAL and OCULAR LARVA MIGRANS
============================================================
1.) Souvenir from the Hamptons - a case of cutaneous larva migrans of six months' duration.
2.) Effectiveness of a new therapeutic regimen with albendazole in cutaneous larva migrans.
3.) [Migrant erythema as clinical presentation of cutaneous larva migrans in Mexico City]
4.) Larva migrans within scalp sebaceous gland.
5.) Cutaneous larva migrans, sacroileitis, and optic neuritis caused by an unidentified organism acquired in Thailand.
6.) Perianal cutaneous larva migrans in a child.
7.) [Infections with Baylisascaris procyonis in humans and raccoons]
8.) Cutaneous larva migrans complicated by erythema multiforme [see comments]
9.) Cutaneous larva migrans associated with water shoe use.
10.) Cutaneous larva migrans infection in the pediatric foot. A review and two case reports.
11.) Creeping eruption of larva migrans--a case report in a beach volley athlete.
12.) Albendazole: a new therapeutic regimen in cutaneous larva migrans.
13.) A primary health care approach to an outbreak of cutaneous larva migrans.
14.) Autochthonous cutaneous larva migrans in Germany.
15.) High prevalence of Ancylostoma spp. infection in dogs, associated with endemic focus of human cutaneous larva migrans, in Tacuarembo, Uruguay.
16.) Persistent cutaneous larva migrans due to Ancylostoma species.
17.) [A case of Dirofilaria repens migration in man]
18.) [Cutaneous larva migrans, autochthonous in France. Apropos of a case]
19.) Cutaneous larva migrans in travelers: synopsis of histories, symptoms, and treatment of 98 patients.
20.) [Nematode larva migrans. On two cases of filarial infection]
21.) Larva migrans that affect the mouth.
22.) Immunological studies on human larval toxocarosis.
23.) [Larva migrans]
24.) Effect of albendazole on Ancylostoma caninum larvae migrating in the muscles of mice.
25.) [Ocular manifestations of toxocariasis]
26.) Toxocara infestations in humans: symptomatic course of toxocarosis correlates significantly with levels of IgE/anti-IgE immune complexes.
27.) [Long-term observations of ocular toxocariasis in children and youth]
28.) [A case of uveitis due to gnathostoma migration into the vitreous cavity]
29.) [The ocular form of toxocariasis]
30.) [Visceral larval migrans (Human toxocariasis) cause of hypereosinophilia and visceral granulomas in adults]
31.) Visceral larva migrans syndrome complicated by liver abscess.
32.) Visceral larva migrans and tropical pyomyositis: a case report.
33.) [2 cases of toxocariasis (visceral larva migrans)]
34.) [Visceral larva migrans. A rare cause of eosinophilia in adults]
35.) [Visceral larva migrans: a mixed form of presentation in an adult. The clinical and laboratory aspects]
36.) Visceral larva migrans induced eosinophilic cardiac pseudotumor: a cause of sudden death in a child.
37.) [Toxocariasis. A cosmopolitan parasitic zoonosis]
38.) Visceral larva migrans mimicking rheumatic diseases.
39.) Hepatic granulomas due to visceral larva migrans in adults: appearance on US and MRI.
40.) [Ascaridiasis zoonoses: visceral larva migrans syndromes]
41.) Hepatic visceral larva migrans: evolution of the lesion, diagnosis, and role of high-dose albendazole therapy.
42.) Neuroimaging studies of cerebral "visceral larva migrans" syndrome. 43.)[Acute eosinophilic pneumonia and the larva migrans syndrome: apropos of a case in an adult]
44.)Toxocariasis simulating hepatic recurrence in a patient with Wilms' tumor.
45.) Hepatic imaging studies on patients with visceral larva migrans due to probable Ascaris suum infection.
46.) Encephalopathy caused by visceral larva migrans due to Ascaris suum.
47.) [Imported skin diseases (see comments)]
48.) [Incidence of Toxocara ova--especially ova of visceral larva migrans
in beach sand of Warnemunde in 1997]
49.) Pets and Parasites.
50.) Cutaneous larva migrans in travelers: synopsis of histories, symptoms, and treatment of 98 patients.
51.) Cutaneous larva migrans.
52.)[Current therapeutic possibilities in cutaneous larva migrans]
53.) Cutaneous larva migrans due to Pelodera strongyloides.
54.) Oral albendazole for the treatment of cutaneous larva migrans.
55.) Cutaneous larva migrans in northern climates. A souvenir of your dream vacation.
56.) Creeping eruption. A review of clinical presentation and management of
60 cases presenting to a tropical disease unit.
57.) Dermatoses associated with travel to tropical countries: a prospective study of the diagnosis and management of 269 patients presenting to a tropical disease unit.
58.) Larva currens and systemic disease.
59.) Hookworm folliculitis.
60.) [Prurigo and further diagnostically significant skin symptoms in strongyloidosis]
61.) Gnathostomiasis, or larva migrans profundus.
62.) Visceral larva migrans caused by Trichuris vulpis.
63.) Creeping disease due to larva of spiruroid nematoda.
64.) Creeping eruption due to larvae of the suborder Spirurina--a newly
recognized causative parasite.
65.) Linear lichen planus mimicking creeping eruption.
66.) Diagnosis and management of Baylisascaris procyonis infection in an infant with nonfatal meningoencephalitis.
67.) [Human gnathostomiasis. The first evidence of the parasite in South America]
68.) Efficacy of ivermectin in the therapy of cutaneous larva migrans
[letter]
69.) Hookworm-related cutaneous larva migrans in northern Brazil:
resolution of clinical pathology after a single dose of ivermectin.
70.) session of carbon dioxide laser: a study of 0.1111/jocd.12296. [Epub ahead of print]
ten cases in the Philippines.
71.) Treatment of 18 children with scabies or cutaneous larva migrans using ivermectin.
============================================================
70.) session of carbon dioxide laser: a study of 0.1111/jocd.12296. [Epub ahead of print]
ten cases in the Philippines.
71.) Treatment of 18 children with scabies or cutaneous larva migrans using ivermectin.
============================================================