El Molusco Contagioso, Origen y tratamientos. !
The Molluscum Contagiosum, Origin and Treatments. !
EDITORIAL ESPAÑOL
==================
Hola amigos de la red, DERMAGIC EXPRESS con nuevo tema de interés, EL
MOLUCO CONTAGIOSO, REVISIÓN, una enfermedad VIRAL causada por un virus
del tipo (ADN) POXVIRUS, familia POXVIRIDAE, género MOLLUSCIPOX.
Es importante que sepas que EL MOLUSCO CONTAGIOSO (MCV) es la tercera
infección cutánea mes frecuente en los niños y está ubicada en el 5TO
lugar entre las enfermedades más frecuentes en TODO EL MUNDO, la cual es
totalmente benigna pero a veces su tratamiento es todo un reto en la
dermatología.
La enfermedad aparece con unas "PÁPULAS" en forma de cúpula con
umbilicación central, de color "PERLADO" o color piel, en cualquier área
del cuerpo: cara, tronco extremidades y región genital. Luego de
aparecer la primera lesión, comienzan a aparecer otras formado grupos o
aisladas en distintas partes del cuerpo. Las lesiones por lo general no
molestan, en ocasiones provocan prurito, provocando un eczema o
irritación en el área donde están localizadas.
Ocasionalmente se puede presentar en las membranas mucosas según
algunos estudios. Nunca he visto un MOLUSCO CONTAGIOSO en mucosas.
!
El virus del MOLUSCO CONTAGIOSO (MCV) tiene 4 variantes o subtipos:
MCV-1 a -4; el tipo MCV-1 es el más común y el tipo MCV-2 se ve por lo
general en adultos. Para él año 2.010 se estimo un total de 122 millones
de personas afectadas en TODO EL MUNDO, 1.8% de la población.
Histopatológicamente (BIOPSIA) las lesiones muestran unos cuerpos de
inclusión denominados CUERPOS DEL MOLUSCO O CUERPOS DE
HENDERSON-PATERSON, los cuales contienen las partículas virales.
El nombre de "MOLUSCO" no viene de los moluscos del mar, es importante
que sepas eso, el nombre se le dio, por la "FORMA" histopatología que
tiene este virus el cual se asemeja a un "MOLUSCO" es por eso que causa
tanta confusión en las personas que van a la consulta.
Y es "CONTAGIOSO" porque si se contagia de persona a persona. De hecho
el mecanismo de contagio de esta enfermedad es el contacto directo con
personas y objetos contaminados como telas, ropa interior, camisas,
pantalones, bordes de piscinas, arena de la playa. De todos estos los
más comunes son: PISCINAS, EL MAR Y EL CONTACTO DIRECTO ENTRE PERSONAS.
Con respecto a su manifestación clínica y GRUPOS DE EDAD, podemos
distinguir 3 grupos de afectados:
1.) LOS NIÑOS: entre 1 año y 11 años de edad, que representan la mayoría de los
casos. Las lesiones se presentan en cualquier área del cuerpo incluido
región genital y perianal, el contagio: otros niños, piscinas, playas,
objetos contaminados.
2.) ADOLESCENTES Y ADULTOS: a través de relaciones sexuales, las lesiones se ubican
principalmente en la región genital.
Es importante que sepas que el MOLUSCO CONTAGIOSO está incluido dentro
de las ENFERMEDADES POR TRANSMISION SEXUAL (ETS), como te dije
adolescentes y adultos.
3.) PACIENTES INMUNODEPRIMIDOS (SIDA): el 10-30% de los pacientes con SIDA presentan molusco contagioso, y
las lesiones son atípicas, muy grandes, siendo denominado MOLUSCO GIGANTE.
El tratamiento como te dije es todo un reto: el método mas utilizado y
tradicional es el CURETAJE (raspado) de las lesiones, pero este en los
niños causa un "GRAN RECHAZO" porque es un método invasivo y doloroso.
En áreas como la cara y genital NO ES BUENO UTILIZAR EL CURETAJE porque
puedes dejar "MARCADO" al niño.
Es aquí donde entra la "ESTRATEGIA" DEL MEDICO para eliminar el
molusco de la mejor manera posible y sin dolor en los niños: para ello
existen numerosos productos los cuales te coloque en la
lista.
En mi experiencia los más efectivos y menos lesivos para los niños
son: crema de ACIDO RETINOICO AL 0.05% una vez en las noches en las
lesiones. Crema con ACIDO SALICILICO Y ACIDO LACTICO en bajas
concentraciones una vez en el día. Pero obviamente cada dermatólogo
tiene su método.
Particularmente LOS PRODUCTOS CÁUSTICOS como IMIQUIMOD, ACIDO
SALICILICO, ACIDO LACTICO, PODOFILINA y otros a altas concentraciones,
probablemente eliminen el molusco, pero quedaran marcas secuela en la
piel. En región GENITAL no deben ser utilizados.
De hecho hay estudios donde se demuestra que el MOLUSCO CONTAGIOSO,
desaparece espontáneamente con el tiempo, o luego de ser "EXTRAIDA"
una o varias lesiones. Esto te lo cuento porque las madres se
"DESESPERAN" por la presencia de estas lesiones y recurren al CURETAJE
O CAUSTICOS dejando al niño "marcado".
Existe un método sencillo que es "pellizcar" las lesiones hasta
extraer el contenido, algunos pacientes utilizan esta alternativa. y
luego colocan una crema con esteroide y antibiotico para terminar de
sanar la lesión extraída.
En los adolescentes y adultos con localización genital el
MÉTODO DE ELECCIÓN y más efectivo es el CURETAJE de las
lesiones.
En los pacientes con SIDA los métodos incluyen uso INTRALESIONAL,
TOPICO E INTRAVENOSO.
====================================================
1.) CURETAJE.
2.) CRIOTERAPIA.
3.) IMIQUIMOD 1%, O 5% (TOPICO)
4.) CIMETIDINA ORAL.
5 .) GRISEOFULVINA ORAL.
6.) GEL DE ACIDO SALICILICO. (TOPICO).
7.) TRETINOIN 0,05% (ACIDO RETINOICO) TOPICO.
8.) ACIDO LACTICO. (TOPICO).
9.) SOLUCION DE HIDROXIDO DE POTASIO ( KOH 2,5, 5, 10, 15 Y 20%) TÓPICO.
10.) ANTIGENO DE CANDIDA (INTRALESIONAL).
11.) CANTARIDINA (TOPICO).
12.) CREMA DE PODOFILOTOXINA (0,3-0,5%).
13.) PASTA DE NITRATO DE PLATA (40%) TOPICA).
14.) ACEITE ESENCIAL DE MIRTO DE LIMON AUSTRALIANO (BACKHOUSIA CITRIODORA) TOPICO.
15.) TINTURA DE YODO (10%) TOPICA.
16.) ADAPALENO (TOPICO).
17.) NITRITO DE SODIO (5%) TOPICO.
18.) LASER PULSADO (588 nm).
19.) INMUNOTERAPIA INTRALESIONAL CON VACUNA MMR (SARFAMPION, PAPERA Y RUBEOLA).
20.) DIPFENCIPRONA (IMMUNOTERAPIA).
21.) SOLUCIÓN DE FENOL.
22.) CIDOFOVIR (TOPICO INTRALESIONAL, INTRAVENOSO).
Para finalizar te digo que con EL MOLUSCO CONTAGIOSO la
estrategia final debe ser eliminarlo sin dejar "MARCADO" al paciente,
en el caso de los niños.
Debes elegir un método, el que más te guste, pero sin dejar
secuelas en la piel, pues es bien sabido que en los niños TARDE O
TEMPRANO las lesiones desaparecerán.
Saludos a todos.
Dr. José lapenta.
Dr. José M. lapenta.
EDITORIAL ENGLISH
==================
Hello friends of the network, DERMAGIC EXPRESS with new topic of
interest, THE MOLLUSCUM CONTAGIOSUM, A REVIEW: VIRAL disease caused by
a virus of the type (DNA) POXVIRUS, family POXVIRIDAE, genus
MOLLUSCIPOX.
It is important that you know that MOLLUSCUM CONTAGIOSUM (MCV) is the
third most frequent skin infection in children and is located in the
5th place among the most frequent diseases in ALL THE WORLD, which is
totally benign but sometimes its treatment is a challenge in
dermatology.
The disease appears with a PAPULES dome shaped, with central
umbilitation" of "PEARL"color or SKIN color, in any area of the
body: face, trunk extremities and genital region. After the first
lesion appears, other formed groups or isolated in different parts of
the body begin to appear. The lesions usually do not disturb,
sometimes provoke pruritus, causing eczema or irritation in the area
where they are located.
Occasionally it may present in mucous membranes according to some
studies: I have never seen a MOLLUSCUM CONTAGIOSUM in oral, genital or
anal mucosa.
MOLLUSCUM CONTAGIOSUM virus (MCV) has 4 variants or subtypes: MCV-1 to
-4; The MCV-1 type is the most common and the MCV-2 type is usually
seen in adults. For the year 2010, a total of 122 million people were
affected ALL OVER THE WORLD, 1.8% of the population.
Histopathologically (BIOPSY) the lesions show inclusion bodies called
MOLLUSCUM BODIES OR HENDERSON-PATERSON BODIES, which contain the viral
particles.
The name "MOLLUSCUM " does not come from the mollusks of the sea, it
is important that you know that, the name was given, by the
histopathology "FORM" that has this virus which resembles a "MOLLUSK"
that is why So much confusion in the people who go to the
consultation.
And it is "CONTAGIOSUM " because it is spread from person to person.
In fact the mechanism of contagion of this disease is the direct
contact with people and objects contaminated like cloths, underwear,
shirts, pants, borders of swimming pools, sand of the beach. Of all
these the most common are: SWIMMING POOLS, THE SEA AND THE DIRECT
CONTACT AMONG PEOPLE.
With respect to its clinical manifestation and AGE GROUPS, we can
distinguish 3 affected groups:
1.) CHILDREN: between 1 year and 11 years of age, representing the majority of
cases.
Lesions occur in any area of the body including genital and perianal
region, contagion: other children, swimming pools, beaches,
contaminated objects.
2.) ADOLESCENTS AND ADULTS:
through sexual relations, the lesions are located mainly in the
genital region.
It is important that you know that the MOLLUSCUM CONTAGIOSUM is
included in SEXUAL TRANSMISSION DISEASES (ETS), as I told you,
teenagers and adults.
3.) PATIENTS WITH IMMUNODEFICIENCY (AIDS):
10-30% of patients with AIDS present molluscum contagiosum, and the
lesions are atypical, very large, being denominated
GIANT MULLUSCUM.
The treatment as I told you is a challenge: the most used and
traditional method is the CURETTAGE (scraping) of the lesions, but
this in children causes a "GREAT REJECTION" because it is an invasive
and painful method. In areas such as the face and genital it is not
good to use the curettage because you can leave the child
"MARKED".
This is where the "STRATEGY" OF THE DOCTOR enters to eliminate the
MOLLUSCUM in the best possible and painless way in children: for this,
there are numerous products which will put you on the list.
In my experience the most effective and least harmful for children
are: RETINOIC ACID cream 0.05% once at night in the lesions. Cream
with salicylic acid and lactic acid in low concentrations once in the
day. But obviously every dermatologist has his method.
Particularly CAUSTIC PRODUCTS such as IMIQUIMOD, SALICYLIC ACID,
LACTIC ACID, PODOPHYLINE and others at high concentrations will
probably eliminate the molluscum, but there will be sequelae marks on
the skin. In GENITAL region should not be used.
In fact there are studies where it is shown that the MOLLUSCUM
CONTAGIOSUM disappears spontaneously with time, or after being
"EXTRACTED" one or more lesions. This I tell you because mothers are
"DESPERATE" because of the presence of these lesions and choose the
CURETTAGE or CAUSTIC leaving the skin child "marked".
There is a simple method that is "pick" and scratch the lesions until
the content is extracted, some patients use this alternative. And then
put a cream with steroid and antibiotic to finish healing the lesion
extracted.
In adolescents and adults with genital localization the METHOD OF
ELECTION and more effective is the CURETTAGE of the lesions.
In patients with AIDS the methods include INTRALESIONAL, TOPIC AND
INTRAVENOUS use.
TREATMENTS USED FOR MOLLUSCUM CONTAGIOSUM:
================================================
1.) CURETTAGE.
2.) CRYOTHERAPHY.
3.) IMIQUIMOD 1%, OR 5% (TOPICAL)
4.) ORAL CIMETIDINE.
5..) ORAL GRISEOFULVINE.
6.) SALICYLIC ACID GEL. (TOPICAL)
7.) TRETINOIN 0.05% (RETINOIC ACID) TOPICAL.
8.) LACTIC ACID. (TOPICAL).
9.) POTASSIUM HYDROXIDE SOLUTION (2.5, 5, 10, 15 AND 20%)
TOPICAL.
10.) CANDIDA ANTIGEN (INTRALESIONAL).
11.) CANTHARIDIN (TOPICAL).
12.) PODOPHYLLOTOXIN CREAM (0,3-0,5%).
13.) SILVER NITRATE PASTE (40%) TOPICAL).
14.) ESSENTIAL OIL OF AUSTRALIAN LEMON MYRTLE(BACKHOUSIA CITRIODORA)
TOPICAL.
15.) TINCTURE OF IODINE (10%) TOPICAL.
16.) ADAPALENE (TOPICAL).
17.) SODIUM NITRITE (5%) TOPICAL.
18.) PULSED DYE LASER (588 nm).
19.) INTRALESIONAL IMMUNOTHERAPY WITH MMR VACCINE (MEASLES, MUMPS
AND RUBELLA).
20.) DIPHENCYPRONE (IMMUNOTHERAPHY).
21.) PHENOL SOLUTION.
22.) CIDOFOVIR (TOPICAL, INTRALESIONAL, INTRAVENOUS).
Finally, I tell you that with THE MOLLUSCUM
CONTAGIOSUM, the final strategy should be to eliminate it without
leaving the patient "MARKED", in the case of children.
You must choose a method, which you like, but without leaving behind
sequels on the skin, as it is well known that in children EARLY or
LATER the lesions will disappear.
Greetings to all.
Dr. José Lapenta.
Dr. José M. Lapenta.
=============================================================
REFRENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
=============================================================
1.) [Molluscum contagiosum--a common but poorly understood "childhood disease" and sexually transmitted illness].
2.) Immune evasion strategies of molluscum contagiosum virus.
3.) Identification and typing of molluscum contagiosum virus in clinical specimens by polymerase chain reaction.
4.) Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study.
5.) [THE DIFFERENT PRESENTATIONS OF PERIOCULAR MOLLUSCUM CONTAGIOSUM].
6.) Molluscum contagiosum and associations with atopic eczema in children: a retrospective longitudinal study in primary care.
7.) Clinical and Demographic Characteristics of Patients with Molluscum Contagiosum Treated at the University Dermatology Clinic Maribor in a 5-year period.
8.) Molluscum contagiosum: to treat or not to treat? Experience with 170 children in an outpatient clinic setting in the northeastern United States.
9.) Successful treatment of molluscum contagiosum with intralesional immunotherapy by measles, mumps, and rubella vaccine: a report of two cases.
10.) Intralesional immunotherapy with Candida antigen for the treatment of molluscum contagiosum in children.
11.) Congenital molluscum contagiosum: report of four cases and review of the literature.
12.) Molluscum contagiosum virus infection.
13.) Extensive molluscum contagiosum virus infection in a young adult receiving fingolimod.
14.) Rapid detection and typing of Molluscum contagiosum virus by FRET-based real-time PCR.
15.) Seroprevalence of Molluscum contagiosum virus in German and UK populations.
16.) Disparate antiviral responses in Molluscum contagiosum virus-induced skin lesions.
17.) Close relationship between equine and human molluscum contagiosum virus demonstrated by in situ hybridisation.
18.) Topical 20% KOH--an effective therapeutic modality for moluscum contagiosum in children.
19.) Treatment of pediatric molluscum contagiosum with 10% potassium hydroxide solution.
20.) Topical salicylic acid gel as a treatment for molluscum contagiosum in children.
21.) Essential oil of Australian lemon myrtle (Backhousia citriodora) in the treatment of molluscum contagiosum in children.
22.) Modified curettage technique for molluscum contagiosum.
23.) Curettage treatment for molluscum contagiosum: a follow-up survey study.
24.) An open, comparative study of 10% potassium hydroxide solution versus salicylic and lactic acid combination in the treatment of molluscum contagiosum in children.
25.) Comparative study of 5 % potassium hydroxide solution versus 0.05% tretinoin cream for Molluscum Contagiosum in children.
26.) A comparative study of 10% KOH solution and 5% imiquimod cream for the treatment of Molluscum contagiosum in the pediatric age group.
27.) Comparative study on the efficacy, safety, and acceptability of imiquimod 5% cream versus cryotherapy for molluscum contagiosum in children.
28.) Topical 0.3% and 0.5% podophyllotoxin cream for self-treatment of molluscum contagiosum in males. A placebo-controlled, double-blind study.
29.) Comparative study of 5% and 2.5% potassium hydroxide solution for molluscum contagiosum in children.
30.) Combination topical treatment of molluscum contagiosum with cantharidin and imiquimod 5% in children: a case series of 16 patients.
31.) Topical treatment of molluscum contagiosum with imiquimod 5% cream in Turkish children.
32.) Treatment of molluscum contagiosum with cantharidin: a practical approach.
33.) Treatment of molluscum contagiosum with oral cimetidine: clinical experience in 13 patients.
34.) Treatment of molluscum contagiosum: a brief review and discussion of a case successfully treated with adapelene.
35.) Interventions for cutaneous molluscum contagiosum.
36.) Giant Molluscum Contagiosum in an HIV positive patient.
37.) Giant molluscum contagiosum: an unusual presenting complaint of paediatric HIV disease.
38.) Generalized molluscum contagiosum in an HIV patient treated with diphencyprone.
39.) Molluscum contagiosum effectively treated with a topical acidified nitrite, nitric oxide liberating cream.
40.) Treatment of molluscum contagiosum with silver nitrate paste.
41.) Efficacy of pulsed dyed laser (585 nm) in the treatment of molluscum contagiosum subtype 1.
42.) Oral griseofulvin therapy in molluscum contagiosum.
43.) [Molluscum contagiosum treated by topical using 10% tincture of iodine].
44.) Topical and intralesional cidofovir: a review of pharmacology and therapeutic effects. =======================================================
=======================================================
1.) [Molluscum contagiosum--a common but poorly understood "childhood disease" and sexually transmitted illness].
=======================================================
Med Monatsschr Pharm. 2013 Aug;36(8):282-90.
[Article in German]
Stock I1.
Author information
1
Institut für Medizinische Mikrobiologie, Immunologie und Parasitologie, Abteilung Pharmazeutische Mikrobiologie, Universität Bonn, Bonn. Ingo_Stock@web.de
Abstract
Molluscum contagiosum is a viral disease of the skin characterized by discrete, multiple, flesh-colored papules. It is caused by a highly infectious, enveloped deoxyribonucleic acid virus, called molluscum contagiosum virus (MCV). Molluscum contagiosum is very common in children, sexually active adults and immunocompromised patients, especially those who are infected with the human immunodeficiency virus. MCV transmission usually takes place through direct skin-to-skin contact. Infections in childhood are often linked to swimming-pool attendance. Adults are infected usually through sexual contact. An intimate skin-to-skin contact is sufficient for transmission of the virus. In immunocompetent adults, the warts remain in the genital area and adjacent regions of the skin. In children and patients with immunocompromised conditions, however, various regions of the body are usually affected. Therapy of molluscum contagiosum should be undertaken in an individualized manner, a specific treatment does not exist. For the treatment, physical methods such as curettage and cryotherapy, topic acids (e. g., acetic acid) and alkalis (e. g., potassium hydroxide), some other topical agents such as cantharidin and imiquimod, as well as several systemic agents the pharmacological treatments is, however, sparse. Effective prevention is problematic due to the high infectivity of the virus. A vaccine is not available.
==========================================================
2.) Immune evasion strategies of molluscum contagiosum virus.
==========================================================
Adv Virus Res. 2015;92:201-52. doi: 10.1016/bs.aivir.2014.11.004. Epub 2015 Jan 13.
Shisler JL1.
Author information
1
Department of Microbiology, College of Medicine, University of Illinois, Urbana, Illinois, USA. Electronic address: jshisler@illinois.edu.
Abstract
Molluscum contagiosum virus (MCV) is the causative agent of molluscum contagiosum (MC), the third most common viral skin infection in children, and one of the five most prevalent skin diseases worldwide. No FDA-approved treatments, vaccines, or commercially available rapid diagnostics for MCV are available. This review discusses several aspects of this medically important virus including: physical properties of MCV, MCV pathogenesis, MCV replication, and immune responses to MCV infection. Sequencing of the MCV genome revealed novel immune evasion molecules which are highlighted here. Special attention is given to the MCV MC159 and MC160 proteins. These proteins are FLIPs with homologs in gamma herpesviruses and in the cell. They are of great interest because each protein regulates apoptosis, NF-κB, and IRF3. However, the mechanism that each protein uses to impart its effects is different. It is important to elucidate how MCV inhibits immune responses; this knowledge contributes to our understanding of viral pathogenesis and also provides new insights into how the immune system neutralizes virus infections.
==========================================================
3.) Identification and typing of molluscum contagiosum virus in clinical specimens by polymerase chain reaction.
==========================================================
J Med Virol. 1997 Nov;53(3):205-11.
Thompson CH1.
Author information
1
Department of Infectious Diseases, Faculty of Medicine, University of Sydney, NSW, Australia.
Abstract
A polymerase chain reaction (PCR) which enables the detection of molluscum contagiosum virus (MCV) genomes in either fresh or formalin-fixed clinical specimens is described. The primers used were designed to amplify a 167 bp region of the 3.8 kbp HindIII fragment K of the MCV 1 genome. The ability of this PCR to detect three common MCV types (1, 1v and 2) in clinical specimens was confirmed using frozen extracts from 75 molluscum lesions, and digests of single sections of 11 formalin-fixed, paraffin-embedded lesions; all of which had been previously typed by Southern hybridisation. In addition, 2 specimens previously negative by hybridisation were shown to be positive for MCV DNA by PCR. Confirmation of the identity of the PCR products and distinction between the two major MCV types (MCV 1/1v versus MCV 2) was achieved by comparison of the results of cleavage with the restriction endonucleases Hhal and Sacl. Sequencing of the PCR products revealed complete homology between MCV 1 and 1v, but minor nucleotide variations between MCV 1/1v and MCV 2 were identified. As well as providing a highly sensitive means of diagnosis, the technique may also prove useful for investigations into the pathogenesis, epidemiology and natural history of molluscum contagiosum infection.
==========================================================
4.) Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study.
===========================================================
Lancet Infect Dis. 2015 Feb;15(2):190-5. doi: 10.1016/S1473-3099(14)71053-9. Epub 2014 Dec 23.
Olsen JR1, Gallacher J2, Finlay AY3, Piguet V3, Francis NA2.
Author information
1
Cochrane Institute of Primary Care and Public Health, Cardiff University, Cardiff, Wales, UK. Electronic address: olsenjr@cardiff.ac.uk.
2
Cochrane Institute of Primary Care and Public Health, Cardiff University, Cardiff, Wales, UK.
3
Department of Dermatology and Academic Wound Healing, Institute of Infection and Immunity, Cardiff University and University Hospital of Wales, Cardiff, Wales, UK.
Abstract
BACKGROUND:
Molluscum contagiosum is one of the 50 most prevalent diseases worldwide, but scarce epidemiological data exist for childhood molluscum contagiosum. We aimed to describe the time to resolution, transmission to household child contacts, and effect on quality of life of molluscum contagiosum in children in the UK.
METHODS:
Between Jan 1, and Oct 31, 2013, we recruited 306 children with molluscum contagiosum aged between 4 and 15 years in the UK either by referral by general practitioner or self-referral (with diagnosis made by parents by use of the validated Molluscum Contagiosum Diagnostic Tool for Parents [MCDTP]). All participants were asked to complete a questionnaire at recruitment about participant characteristics, transmission, and quality of life. We measured quality of life with the Children's Dermatology Life Quality Index (CDLQI). Participants were prospectively followed up every month to check on their recovery from molluscum contagiosum and transmission to other children in the same household, until the child's lesions were no longer visible.
FINDINGS:
The mean time to resolution was 13·3 months (SD 8·2). 80 (30%) of 269 cases had not resolved by 18 months; 36 (13%) had not resolved by 24 months. We recorded transmission to other children in the household in 102 (41%) of 250 cases. Molluscum contagiosum had a small effect on quality of life for most participants, although 33 (11%) of 301 participants had a very severe effect on quality of life (CDLQI score >13). A greater number of lesions was associated with a greater effect on quality of life (H=55·8, p<0·0001).
INTERPRETATION:
One in ten children with molluscum contagiosum is likely to have a substantial effect on their quality of life and therefore treatment should be considered for some children, especially those with many lesions or who have been identified as having a severe effect on quality of life. Patients with molluscum contagiosum and their parents need to be given accurate information about the expected natural history of the disorder. Our data provide the most reliable estimates of the expected time to resolution so far and can be used to help set realistic expectations.
FUNDING:
Wales School of Primary Care Research (WSPCR) and Cardiff University.
==========================================================
5.) [THE DIFFERENT PRESENTATIONS OF PERIOCULAR MOLLUSCUM CONTAGIOSUM].
===========================================================
Harefuah. 2015 Nov;154(11):703-7, 742.
[Article in Hebrew]
Zloto O, Rosner M.
Abstract
INTRODUCTION:
Periocular molluscum contagiosum nodules typically appear in a classical presentation. However, the presentation can be different. This makes the diagnosis and the decision on treatment difficult.
AIM:
To report different clinical presentations of periocular molluscum contagiosum and to examine their epidemiological, clinical and histopathological features.
METHODS:
For all patients who were diagnosed with periocular molluscum contagiosum during the years 1995-2014, the following data was extracted from the patients' files: gender, age at the time of diagnosis, location of the lesion, number and dimensions of lesions, clinical presentation, histopathological features, suspected clinical diagnosis before histopathological diagnosis and treatment. A classification according to different presentations was suggested and the epidemiological, clinical and histopathological features of each presentation were examined.
RESULTS:
Molluscum contagiosum was diagnosed in 30 patients: 10 males (33.33%) and 20 females (66.66%). The mean age of diagnosis was 19.3 years old, one patient was immunosuppressive and 29 patients were immunocompetent. Six different clinical presentations were seen: Typical, umbilicated dome shaped lesion (19 cases), big lesion (4 cases), conglomerated lesions (4 cases), erythematous lesion (1 case), inflamed lesion (1 case), and pedunculated lesion (1 case). In all cases the diagnosis was confirmed by histopathological examination and the treatment was surgical excision.
CONCLUSION:
According to this case series of periocular molluscum contagiosum, which is one of the largest published thus far in the ophthalmic literature, six distinct different clinical presentations are suggested. These lesions should be suspected not just in children and in immunosuppressive adult patients but also in immunocompetent patients of all ages.
==========================================================
6.) Molluscum contagiosum and associations with atopic eczema in children: a retrospective longitudinal study in primary care.
==========================================================
Br J Gen Pract. 2016 Jan;66(642):e53-8. doi: 10.3399/bjgp15X688093. Epub 2015 Dec 6.
Olsen JR1, Piguet V2, Gallacher J3, Francis NA4.
Author information
1
Institute of Health and Wellbeing, College of Medical Veterinary and Life Sciences, University of Glasgow, Glasgow.
2
Professor and head of Department of Dermatology and Academic Wound Healing, Division of Infection and Immunity, School of Medicine, Cardiff University, Cardiff.
3
Department of Psychiatry, Medical Sciences Division, University of Oxford, Oxford.
4
Cochrane Institute of Primary Care and Public Health, School of Medicine, Cardiff University, Cardiff.
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is a common skin condition in children. Consultation rates and current management in primary care, and how these have changed over time, are poorly described. An association between the presence of atopic eczema (AE) and MC has been shown, but the subsequent risk of developing MC in children with a diagnosis of AE is not known.
AIM:
To describe the consultation rate and management of MC in general practice in the UK over time, and test the hypothesis that a history of AE increases the risk of developing MC in childhood.
DESIGN AND SETTING:
Two studies are reported: a retrospective longitudinal study of MC cases and an age-sex matched case-cohort study of AE cases, both datasets being held in the UK Clinical Practice Research Datalink from 2004 to 2013.
METHOD:
Data of all recorded MC and AE primary care consultations for children aged 0 to 14 years were collected and two main analyses were conducted using these data: a retrospective longitudinal analysis and an age-sex matched case-cohort analysis.
RESULTS:
The rate of MC consultations in primary care for children aged 0 to 14 years is 9.5 per 1000 (95% CI = 9.4 to 9.6). The greatest rate of consultations for both sexes is in children aged 1-4 years and 5-9 years (13.1 to 13.0 (males) and 13.0 to 13.9 (females) per 1000 respectively). Consultation rates for MC have declined by 50% from 2004 to 2013. Children were found to be more likely to have an MC consultation if they had previously consulted a GP with AE (OR 1.13; 95% CI = 1.11 to 1.16; P<0.005).
CONCLUSION:
Consultations for MC in primary care are common, especially in 1-9-year-olds, but they declined significantly during the decade under study. A primary care diagnosis of AE is associated with an increased risk of a subsequent primary care diagnosis of MC.
==========================================================
7.) Clinical and Demographic Characteristics of Patients with Molluscum Contagiosum Treated at the University Dermatology Clinic Maribor in a 5-year period.
==========================================================
Acta Dermatovenerol Croat. 2016 Jun;24(2):130-6.
Trčko K1, Poljak M, Križmarić M, Miljković J.
Author information
1
Katarina Trčko, MD, Department of Dermatovenereology, University Clinical Centre Maribor, Ljubljanska 5, 2000 Maribor, Slovenia; katarina.trcko@gmail.com.
Abstract
Molluscum contagiosum virus (MCV) is a common skin pathogen in both adults and children. In this prospective study, we clinically evaluated consecutive patients with molluscum contagiosum (MC) who had been examined during a 5-year period at the second-largest dermatology clinic in Slovenia and described their main demographic and clinical characteristics, concomitant diseases, and treatment success. The study included 188 patients, of which 121 (64%) were men and 67 (36%) were women. A total of 135 (72%) patients were adults, with lesions that were most commonly located in the anogenital region (98%) and were probably sexually acquired. Two adult patients were diagnosed with concurrent human immunodeficiency virus (HIV) infection. Fifty-three (28%) patients were children with a mean age of 5.7 years, most commonly presenting with lesions on the torso and extremities (85%). In adults, the infection most commonly occurred in male patients, while in children it was slightly more common in female patients. At presentation, 58% of patients had more than 5 MC lesions. A total of 30% of the included children had concomitant atopic dermatitis. We did not observe an increased occurrence of MCV infection in patients with atopic dermatitis. All patients were treated with curettage of the lesions. The cure rate at the first follow-up visit after 2 months was relatively high (63%), and recurrences were not associated with the number or site of lesions at presentation or with concomitant atopic dermatitis.
==========================================================
8.) Molluscum contagiosum: to treat or not to treat? Experience with 170 children in an outpatient clinic setting in the northeastern United States.
==========================================================
Pediatr Dermatol. 2015 May-Jun;32(3):353-7. doi: 10.1111/pde.12504. Epub 2015 Jan 30.
Basdag H1, Rainer BM1, Cohen BA1.
Author information
1
Division of Pediatric Dermatology, Departments of Pediatrics and Dermatology, Johns Hopkins University School of Medicine, Baltimore, Maryland.
Abstract
Despite the high prevalence of molluscum contagiosum (MC) in children, epidemiologic data on this common self-limited viral infection is limited. In this report we review our experience with the demographic characteristics, clinical characteristics, management, and time to resolution of MC in 170 children. A retrospective medical chart review and telephone survey were conducted on children younger than 16 years of age evaluated for MC in the Division of Pediatric Dermatology at the Johns Hopkins Children's Center, Baltimore, Maryland, from January 1, 2008, to December 31, 2011. Of 170 children with MC, 51.8% were female and 77.1% were Caucasian. The median age at diagnosis was 5 years and 46.5% had a history of atopic dermatitis (AD). Children with AD had significantly more MC lesions than those without (p < 0.05); 72.9% of children did not receive any treatment. MC lesions completely cleared within 12 months in 45.6% of treated and 48.4% of untreated children and within 18 months in 69.5% of treated and 72.6% of untreated children. Treatment (if any), sex, race, diagnosing physician, number of lesions at diagnosis, number of anatomic locations, or history of AD did not predict time to resolution of MC lesions. MC lesions completely resolved in approximately 50% of children within 12 months and in 70% within 18 months. Treatment did not shorten the time to resolution.
==========================================================
9.) Successful treatment of molluscum contagiosum with intralesional immunotherapy by measles, mumps, and rubella vaccine: a report of two cases.
==========================================================
Dermatol Ther. 2014 Nov-Dec;27(6):373-6. doi: 10.1111/dth.12158. Epub 2014 Jul 22.
Na CH1, Kim DJ, Kim MS, Kim JK, Shin BS.
Author information
1
Department of Dermatology, Chosun University Medical School, Gwangju, Korea.
Abstract
Molluscum contagiosum (MC) is a common viral infection of the skin and mucous membrane that often affects young children. Generally, physical removal by surgical curettage is commonly used for the treatment of MC, but the pain during the treatment is a major problem. Thus immunotherapy using various antigens has been introduced recently. Here we present two cases of MC that improved with measles, mumps, and rubella (MMR) vaccine intralesional injection. On the ground of our knowledge, they were the first cases of successful MMR intralesional injection in this disease entity.
==========================================================
10.) Intralesional immunotherapy with Candida antigen for the treatment of molluscum contagiosum in children.
===========================================================
Pediatr Dermatol. 2011 May-Jun;28(3):254-8. doi: 10.1111/j.1525-1470.2011.01492.x.
Enns LL1, Evans MS.
Author information
1
University of Arkansas for Medical Sciences and Arkansas Children's Hospital, USA. lindsayenns@gmail.com
Abstract
Intralesional injection of Candida and other antigens is an established and useful therapy for warts; a cutaneous immune response can induce improvement and or clearance of warts, often with response in anatomically distinct lesions other than those injected. Molluscum contagiosum virus is a common cutaneous infection seen primarily in pediatric dermatology clinics. Treatment is often unsatisfactory, painful, and time consuming. A retrospective chart review was conducted to examine the efficacy of intralesional injection of Candida antigen into a maximum of three individual molluscum lesions. Twenty-nine patients were treated with this therapy; 55% had complete resolution. In addition, 37.9% experienced partial resolution, yielding an overall response rate of 93%. Only two patients failed to respond (6.9%). In addition, only four patients reported a single adverse effect of pain with injection. No other adverse effects were reported or noted clinically. Scarring was absent. No recurrences were reported at the time of publication. This report establishes the efficacy of intralesional injection of Candida for
==========================================================
11.) Congenital molluscum contagiosum: report of four cases and review of the literature.
==========================================================
Pediatr Dermatol. 2008 Sep-Oct;25(5):553-6. doi: 10.1111/j.1525-1470.2008.00730.x.
Connell CO1, Oranje A, Van Gysel D, Silverberg NB.
Author information
1
Department of Dermatology, St. Luke's-Roosevelt Hospital Center, New York, New York 10025, USA.
Abstract
Molluscum contagiosum is a viral infection of the skin and mucous membranes that is caused by infection with the molluscum contagiosum virus. Molluscum contagiosum can be acquired from skin to skin contact which may be during play, in a swimming pool, or through sexual contact. Sexually acquired molluscum is rare in younger children, but becomes quite common during adolescence and young adulthood, after the sexual debut. It has been long known that the human papillomavirus, which causes genital warts, i.e., condyloma accuminatum, can be vertically transmitted through an infected genital tract. Children may not manifest condyloma lesions for a few years. The entity of congenital molluscum has been debated in the literature and only three cases of suspected congenital molluscum have been reported. We report on four more infants with congenital molluscum, two children with congenital lesions, and two children with onset of lesions at 6 weeks of age. Two children had single cutaneous lesions on the extremities and two had lesions of the scalp consistent with the site of cervical pressure. Congenital molluscum appears to be a more common entity than previously reported. Vertical transmission of molluscum should be considered for all infantile cases of molluscum.
==========================================================
12.) Molluscum contagiosum virus infection.
==========================================================
Chen X1, Anstey AV, Bugert JJ.
Author information
1
Department of Dermatology, Ruijin Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China.
Abstract
Molluscum contagiosum virus is an important human skin pathogen: it can cause disfigurement and suffering in children, in adults it is less common and often sexually transmitted. Extensive and persistent skin infection with the virus can indicate underlying immunodeficiency. Traditional ablative therapies have not been compared directly with newer immune-modulating and specific antiviral therapies. Advances in research raise the prospect of new approaches to treatment informed by the biology of the virus; in human skin, the infection is localised in the epidermal layers, where it induces a typical, complex hyperproliferative lesion with an abundance of virus particles but a conspicuous absence of immune effectors. Functional studies of the viral genome have revealed effects on cellular pathways involved in the cell cycle, innate immunity, inflammation, and cell death. Extensive lesions caused by molluscum contagiosum can occur in patients with DOCK8 deficiency-a genetic disorder affecting migration of dendritic and specialised T cells in skin. Sudden disappearance of lesions is the consequence of a vigorous immune response in healthy people. Further study of the unique features of infection with molluscum contagiosum virus could give fundamental insight into the nature of skin immunity.
==========================================================
13.) Extensive molluscum contagiosum virus infection in a young adult receiving fingolimod.
==========================================================
Mult Scler. 2016 Jun;22(7):969-71. doi: 10.1177/1352458516629560. Epub 2016 Feb 9.
Behle V1, Wobser M2, Goebeler M2, Stoevesandt J2.
Author information
1
Department of Dermatology, Venerology and Allergology, University Hospital of Würzburg, Würzburg, Germany Behle_V@ukw.de.
2
Department of Dermatology, Venerology and Allergology, University Hospital of Würzburg, Würzburg, Germany.
Abstract
Fingolimod-related viral infections have been described on several occasions since its introduction in 2010. We hereby add a report on an otherwise immunocompetent, 18-year old Caucasian man with relapsing-remitting multiple sclerosis who developed a protracted and extensive molluscum contagiosum (MC) virus infection shortly after being started on fingolimod. Wide-spread cutaneous MC infections in adult patients are considered indicative of underlying immunosuppression. Neurologists prescribing fingolimod ought to be aware of a possibly increased risk of MC, but also need to know about its relative benignity, lack of extra-cutaneous complications, and adequate treatment options.
==========================================================
14.) Rapid detection and typing of Molluscum contagiosum virus by FRET-based real-time PCR.
==========================================================
J Virol Methods. 2013 Feb;187(2):431-4. doi: 10.1016/j.jviromet.2012.11.008. Epub 2012 Nov 20.
Hošnjak L1, Kocjan BJ, Kušar B, Seme K, Poljak M.
Author information
1
Institute of Microbiology and Immunology, Faculty of Medicine, University of Ljubljana, Ljubljana, Slovenia.
Abstract
A fluorescence resonance energy transfer (FRET)-based real-time PCR (RT-PCR) was developed for very sensitive and specific detection of Molluscum contagiosum virus (MCV), as well as reliable differentiation of the two MCV subtype genetic lineages, MCV1 and MCV2, in a single reaction. The assay employs modified primers specific for the viral MC021L gene and uses two novel FRET hybridization probes to detect polymorphisms specific for each of the two subtypes. The sensitivity of the assay at a 95% detection level for both MCV subtypes was 3.3 DNA copies/reaction and the dynamic range was nine orders of magnitude, discriminating 10-10(9) viral genome equivalents/reaction. Post-amplification probe-specific dissociation analysis differentiated the two viral subtypes reliably in all tested concentrations. Testing of 43 tissue specimens clinically diagnosed as MCV lesions showed complete agreement with the results obtained with previously described MCV specific MC080R Taqman RT-PCR and MC021L whole gene sequencing. The novel assay is simple, robust and easy to perform, and may be of great value for clinical and epidemiological studies of MCV infections and related conditions.
==========================================================
15.) Seroprevalence of Molluscum contagiosum virus in German and UK populations.
==========================================================
PLoS One. 2014 Feb 18;9(2):e88734. doi: 10.1371/journal.pone.0088734. eCollection 2014.
Sherwani S1, Farleigh L1, Agarwal N2, Loveless S3, Robertson N3, Hadaschik E4, Schnitzler P5, Bugert JJ1.
Author information
1
Cardiff University School of Medicine, Institute of Infection and Immunity/Medical Microbiology, Cardiff, United Kingdom.
2
Dr P N Behl Skin Institute and School of Dermatology, New Delhi, India.
3
Cardiff University Medical School, Institute of Psychological Medicine and Clinical Neuroscience, Cardiff, United Kingdom.
4
Universität Heidelberg, Hautklinik, Heidelberg, Germany.
5
Universität Heidelberg, Dept.of Infectious Diseases, Heidelberg, Germany.
Abstract
Molluscum contagiosum virus (MCV) is a significant but underreported skin pathogen for children and adults. Seroprevalence studies can help establish burden of disease. Enzyme linked immunosorbent assay (ELISA) based studies have been published for Australian and Japanese populations and the results indicate seroprevalences between 6 and 22 percent in healthy individuals, respectively. To investigate seroprevalence in Europe, we have developed a recombinant ELISA using a truncated MCV virion surface protein MC084 (V123-R230) expressed in E. coli. The ELISA was found to be sensitive and specific, with low inter- and intra-assay variability. Sera from 289 German adults and children aged 0-40 years (median age 21 years) were analysed for antibodies against MC084 by direct binding ELISA. The overall seropositivity rate was found to be 14.8%. The seropositivity rate was low in children below the age of one (4.5%), peaked in children aged 2-10 years (25%), and fell again in older populations (11-40 years; 12.5%). Ten out of 33 healthy UK individuals (30.3%; median age 27 years) had detectable MC084 antibodies. MCV seroconversion was more common in dermatological and autoimmune disorders, than in immunocompromised patients or in patients with multiple sclerosis. Overall MCV seroprevalence is 2.1 fold higher in females than in males in a UK serum collection. German seroprevalences determined in the MC084 ELISA (14.8%) are at least three times higher than incidence of MC in a comparable Swiss population (4.9%). While results are not strictly comparable, this is lower than Australian seroprevalence in a virion based ELISA (n = 357; 23%; 1999), but higher than the seroprevalence reported in a Japanese study using an N-terminal truncation of MC133 (n = 108, 6%; 2000. We report the first large scale serological survey of MC in Europe (n = 393) and the first MCV ELISA based on viral antigen expressed in E. coli.
==========================================================
16.) Disparate antiviral responses in Molluscum contagiosum virus-induced skin lesions.
==========================================================
J Invest Dermatol. 2011 Feb;131(2):288-90. doi: 10.1038/jid.2010.368.
Swiecki M1, Colonna M.
Author information
1
Department of Pathology and Immunology, Washington University School of Medicine, St Louis, Missouri 63110, USA.
Abstract
Molluscum contagiosum virus (MCV) is a poxvirus that causes tumor-like skin lesions. New evidence indicates that plasmacytoid dendritic cells, type I interferon production, and interferon-induced dendritic cells have prominent roles in anti-MCV responses, and these features characterize the inflammatory response in lesions that will likely undergo spontaneous regression.
==========================================================
17.) Close relationship between equine and human molluscum contagiosum virus demonstrated by in situ hybridisation.
==========================================================
Thompson CH1, Yager JA, Van Rensburg IB.
Author information
1
Department of Infectious Diseases, Faculty of Medicine, The University of Sydney, Australia.
Abstract
To determine whether the virus responsible for human molluscum contagiosum (MCV) is the causal agent of a similar disease in horses, in situ hybridisations using cloned fragments of human MCV DNA labelled with digoxigenin were carried out on formalin-fixed biopsy sections of lesions from two horses with molluscum contagiosum-like skin lesions. In both instances there was evidence of specific hybridisation of the labelled probe to target DNA in the sections under high stringency conditions, identified by the development of a deep blue-purple stain in the cytoplasm of cells in the stratum spinosum and stratum granulosum of the lesions and the absence of non-specific hybridisation in adjacent non-lesional areas of the epidermis. These results indicate that on the basis of very close homology of their viral DNA sequences, the causative virus of equine molluscum contagiosum is either identical with, or very closely related to, its human equivalent.
==========================================================
18.) Topical 20% KOH--an effective therapeutic modality for moluscum contagiosum in children.
==========================================================
Indian J Dermatol Venereol Leprol. 2003 Mar-Apr;69(2):175-7.
Mahajan BB1, Pall A, Gupta RR.
Author information
1
Dept. of Dermatology, Govt. Medical College & Hospital, Faridhot, Punjab.
Abstract
Topically 20% KOH aqueous solution once daily at bedtime was applied in 27 children having molluscum contagiosum by their parents, till lesions showed signs of inflammation or superficial ulceration. 24 children (88.9%) completed the trial and complete clearance was achieved after a mean period of 17 days. No recurrence was observed during follow up period. Thus in this open trial topical 20% KOH aqueous solution has proved to be convenient, easy to apply at home, safe and inexpensive alternative therapeutic modality for the treatment of molluscum contagiosum in children.
==========================================================
19.) Treatment of pediatric molluscum contagiosum with 10% potassium hydroxide solution.
==========================================================
J Dermatolog Treat. 2014 Jun;25(3):246-8. doi: 10.3109/09546634.2012.697988. Epub 2012 Jul 25.
Can B1, Topaloğlu F, Kavala M, Turkoglu Z, Zindancı I, Sudogan S.
Author information
1
Department of Dermatology, University of Medeniyet Goztepe Training and Research Hospital , Istanbul , Turkey.
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is a common cutaneous viral infection of the skin that is frequently seen in children. Although lesions can resolve spontaneously, treatment is mandatory because of the psychological effect of widespread lesions in children. Potassium hydroxide (KOH) is a strong alkali that has been used by dermatologists for a long time in identifying the fungal infections from skin scrapings.
AIMS:
We evaluated 40 children with MC for the safety and efficacy of treatment with topical 10% KOH aqueous solution.
METHODS:
Parents were instructed to apply a 10% KOH aqueous solution, twice daily, with a cotton stick to all lesions. Treatment was continued till the lesions showed signs of inflammation or superficial ulceration. Assessments of response and side effects were performed at the end of week 2, week 4, week 8 and week 12.
RESULTS:
We found complete clearance of lesions in 37 (92.5%) patients receiving topical 10%KOH solution after a mean period of four weeks. Three children dropped out of the study; two children reported severe stinging of the lesions and discontinued the treatment; the other patient developed hypopigmentation during the treatment. Local side effects were observed in 12 children (32.4%).
CONCLUSION:
Even though 10% KOH solution is associated with some local side effects, it is a safe, effective, inexpensive and noninvasive alternative treatment of MC in children.
==========================================================
20.) Topical salicylic acid gel as a treatment for molluscum contagiosum in children.
==========================================================
J Dermatolog Treat. 2005;16(5-6):336-40.
Leslie KS1, Dootson G, Sterling JC.
Author information
1
Department of Dermatology, Norfolk & Norwich University Hospital, Norwich, UK. kieronleslie@doctors.org.uk
Abstract
OBJECTIVE:
To determine if the application of salicylic acid gel or phenol solution affected resolution of molluscum contagiosum (MC) lesions in children.
PATIENTS AND METHODS:
This was a randomized, prospective controlled trial with two treatment arms and one vehicle arm for treatment of MC in children. The trial was set in the dermatology outpatient clinics of a teaching hospital and a district general hospital. A total of 114 children were enrolled in the study (age range 1-15 years) over a 4-year period; 83 of the children completed the study. Patients were randomized to receive one of three possible treatments: monthly vehicle application of 70% alcohol, monthly application of 10% phenol in 70% alcohol once or twice weekly 12% salicylic acid gel. All patients also received treatment with daily aqueous cream to reduce eczema. They returned monthly to the clinic for treatment and counting of MC lesions. They were reviewed either until complete resolution or up to 6 months, whichever occurred sooner. The main outcome measure was the time taken for complete resolution of MC lesions.
RESULTS:
In the intention-to-treat analysis there was no difference between treatment arms when the 31 non-completers were analysed as failures (log-rank test: p = 0.38). In an 'as treated' analysis, 16 of 27 children (59.2%: 95% confidence interval 30.2-88.3) had cleared with vehicle, 18 of 32 (56.3%, 30.3-82.2) with phenol solution and 21 of 24 (87.5%, 50.1-124.9) with salicylic acid gel (log-rank test: p = 0.03). On an as treated basis, salicylic acid was significantly better at clearing MC than dilute phenol (p = 0.006). The treatment in all groups was very well tolerated or acceptable in 93% of children.
CONCLUSION:
Our results suggest that topical salicylic acid may be beneficial in speeding resolution of MC in children. Dilute phenol application does not appear to affect the disease course.
==========================================================
21.) Essential oil of Australian lemon myrtle (Backhousia citriodora) in the treatment of molluscum contagiosum in children.
======== ==================================================
Biomed Pharmacother. 2004 May;58(4):245-7.
Burke BE1, Baillie JE, Olson RD.
Author information
1
Cardiovascular Section, Center for Biomedical Research, Inc., 2572 Waterbury lane, Boise, ID 83706-4980, USA. drq10@iglide.net
Abstract
Molluscum contagiosum is a common viral illness of childhood and is increasingly found as a sexually transmitted disease in sexually active young adults. Current treatment options are invasive, requiring tissue destruction and attendant discomfort. Thirty-one children (mean age 4.6 +/- 2.1 years) with the diagnosis of molluscum contagiosum (mean length of time with condition 8.6 +/- 5.3 months) were treated with once daily topical application of a 10% solution (v/v) of essential oil of Australian lemon myrtle (Backhousia citriodora) or vehicle (olive oil). At the end of 21 days, there was greater than 90% reduction in the number of lesions in 9/16 children treated with lemon myrtle oil, while 0/16 children met the same criteria for improvement in the vehicle group (P < 0.05). No adverse events were reported.
==========================================================
22.) Modified curettage technique for molluscum contagiosum.
==========================================================
Pediatr Dermatol. 2007 Mar-Apr;24(2):192-4.
Martín-García RF1, García ME, Rosado A.
Author information
1
Department of Dermatology, Medical Sciences Campus, University of Puerto Rico, Puerto Rico. martinmubarak@aol.com
Abstract
Molluscum contagiosum is a frequently occurring, virally induced cutaneous condition that affects infants, children, and adults. Although historically considered a self-limiting entity, many patients experience prolonged infections, often resistant to varied therapeutic interventions. Topical treatments achieve complete clearance in only a limited number of patients. Because of the associated pain, affected children are characteristically uncompliant to commonly used destructive modalities. We describe a modification of the traditional curettage technique to remove lesions of molluscum contagiosum, which has proven to be effective and well tolerated by a significant number of patients in our practice.
==========================================================
23.) Curettage treatment for molluscum contagiosum: a follow-up survey study.
==========================================================
Simonart T1, De Maertelaer V.
Author information
1
Department of Dermatology, Erasme University Hospital, 808 Route de Lennik, B-1070 Brussels, Belgium. tsimonar@ulb.ac.be
Abstract
BACKGROUND:
Although curettage is commonly used to treat molluscum contagiosum, prospective studies on its effectiveness are lacking.
OBJECTIVES:
To evaluate prospectively the efficacy of curettage in the treatment of molluscum contagiosum and to identify the risk factors associated with treatment failure.
METHODS:
A systematic 2-month follow-up survey study was carried out on 73 patients treated by curettage for molluscum contagiosum.
RESULTS:
Treatment of molluscum contagiosum by curettage was associated with a high risk of treatment failure at week 4 (42/64, 66%) and at week 8 (25/55, 45%). Risk factors for treatment failure at week 4 and 8 were the number of lesions at day 0 (P < 0.001), the number of involved anatomical sites (P < 0.001) and concomitant atopic dermatitis (P = 0.038 and P < 0.001, at weeks 4 and 8, respectively).
CONCLUSIONS:
The main risk factor for treatment failure is lesion number, underlining the importance of the early detection of the lesions or, alternatively, emphasizing the need for therapeutic options other than curettage in patients with numerous lesions.
==========================================================
24.) An open, comparative study of 10% potassium hydroxide solution versus salicylic and lactic acid combination in the treatment of molluscum contagiosum in children.
===========================================================
J Dermatolog Treat. 2013 Aug;24(4):300-4. doi: 10.3109/09546634.2011.649690. Epub 2012 Jan 31.
Köse O1, Özmen İ, Arca E.
Author information
1
Department of Dermatology, Gulhane School of Medicine, Ankara, Turkey. okose@gata.edu.tr
Abstract
OBJECTIVES:
To evaluate and compare the safety and efficacy of 10% potassium hydroxide (KOH) solution and salicylic and lactic acid (SAL + LAC) combination in the treatment of molluscum contagiosum (MC).
MATERIAL AND METHODS:
26 patients with MC randomized into two treatment groups. 12 patients treated with 10% KOH solution and 14 patients treated with SAL + LAC combination for 6 weeks. Parents of patients were instructed to apply medication once daily only to lesions at study onset. Assessment of response of the treated lesions and side effects was performed at 2, 4 and 6 weeks of the treatment. Newly acquired lesions were not included in the study.
RESULTS:
At the end of therapy, 83.3% (n = 10) of KOH group demonstrated complete remission and 16.7% (n = 2) of them showed partial remission; four patients (33%) developed new lesions during the study. All the patients in the SAL + LAC combination group (100%) demonstrated complete remission of study entry lesions at the end of 6 weeks with five patients (35%) acquiring new lesions during the study. Minor side effects were observed in two groups.
CONCLUSIONS:
10% KOH solution and SAL + LAC combination were found to be equally effective in the treatment of MC in children.
==========================================================
25.) Comparative study of 5 % potassium hydroxide solution versus 0.05% tretinoin cream for Molluscum Contagiosum in children.
==========================================================
Kathmandu Univ Med J (KUMJ). 2011 Oct-Dec;9(36):291-4.
Rajouria EA1, Amatya A, Karn D.
Author information
1
Department of Dermatology, Kathmandu University School of Medical Sciences, Dhulikhel Hospital- Kathmandu University Hospital, Dhulikhel, Nepal. eliz_aryal@yahoo.com
Abstract
BACKGROUND:
Molluscum contagiosum is one of the commonest cutaneous viral infections in children. All treatment modalities are associated with substantial pain, tissue destruction, and frequent recurrence.
OBJECTIVES:
To compare the efficacy and side effects of KOH 5% solution with tretinoin 0.05% cream for the treatment of molluscum contagiosum in children.
METHODS:
Fifty patients were randomly divided into 2 groups; 25 each for 5% KOH solution and 0.05% tretinoin cream. The given medication was applied at bed time over molluscum lesions. The assessment of response and side effects were performed weekly for 4 weeks.
RESULTS:
At the end of 4 weeks, the mean lesion count decreased from 9.48 +/- 3.00 SD to 1.67 +/- 0.58 SD and from 8.35 +/- 2.82 SD to 2.00 +/- 1.00 SD in patients treated with 5% KOH solution and 0.05% tretinoin cream respectively.
CONCLUSION:
The result of both KOH and tretinoin showed good response, well tolerated by children but between the two, KOH showed fast recovery and most lesions were resolved before 4 week. The side effects could be minimized if applied as stated above. On the other hand, tretinoin showed delayed response and even some of lesion extended beyond 4 week but the side effect were less, and hence can be used in recurrent cases.
==========================================================
26.) A comparative study of 10% KOH solution and 5% imiquimod cream for the treatment of Molluscum contagiosum in the pediatric age group.
==========================================================
Indian Dermatol Online J. 2015 Mar-Apr;6(2):75-80. doi: 10.4103/2229-5178.153005.
Chathra N1, Sukumar D1, Bhat RM1, Kishore BN1, Martis J1, Kamath G1, Srinath MK1, Monteiro R1.
Author information
1
Department of Dermatology, Venereology and Leprosy, Father Muller Medical College and Hospital, Kankanady, Mangalore, Karnataka, India.
Abstract
BACKGROUND:
Although Molluscum contagiosum (MC) is a self-limiting condition, active therapy could prevent further spread and improve cosmesis. Most of the available treatment modalities traumatize the lesions and have to be undertaken in the hospital, therefore evoking panic in children. In the quest for an alternative therapy, this study comparing 10% potassium hydroxide (KOH) solution and 5% imiquimod cream was taken up.
AIMS AND OBJECTIVES:
To compare the efficacy and tolerability of 10% KOH and 5% imiquimod in the treatment of MC.
MATERIALS AND METHODS:
This comparative study was conducted over a period of 18 months from October 2011 to March 2013, 40 patients between the age group of 1-18 years with clinically diagnosed MC were divided into two groups (lottery method), 20 patients were treated with 5% imiquimod cream (Group A) and the other 20 were treated with 10% KOH solution (Group B). Patients were followed up on the 4(th), 8(th) and 12(th) week of treatment.
RESULTS:
At the end of 12 weeks, out of 20 patients who received 10% KOH, 17 patients showed complete disappearance, whereas out of 20 patients who received 5% imiquimod, only 10 patients showed total clearance of the lesions. Adverse events were more frequent with 10% KOH, pigmentary disturbances being the most common.
CONCLUSION:
With only minor adverse effects, 10% KOH is an inexpensive and efficient modality for the treatment of MC in the pediatric age group. Although 5% imiquimod was effective in clearing the lesions with minimal adverse effects, the longer duration required for its efficacy may deter its wider use.
==========================================================
27.) Comparative study on the efficacy, safety, and acceptability of imiquimod 5% cream versus cryotherapy for molluscum contagiosum in children.
===========================================================
Pediatr Dermatol. 2010 Jul-Aug;27(4):388-94. doi: 10.1111/j.1525-1470.2009.00974.x. Epub 2010 Oct 4.
Al-Mutairi N1, Al-Doukhi A, Al-Farag S, Al-Haddad A.
Author information
1
Department of Dermatology & Venereology, Farwaniya Hospital, Farwaniya, Kuwait. nalmut@usa.net
Abstract
To compare the efficacy, safety and acceptability of imiquimod (IMQ) 5% cream with cryotherapy for the treatment of molluscum contagiosum (MC) in children. Prospective, randomized, comparative, observer blinded study. A total of 74 children, with MC were divided randomly to receive treatment with either IMQ 5% cream (group A) 5 days a week or cryotherapy (group B) once a week until clinical cure or up to a maximum of 16 weeks. All the patients were followed up weekly during active treatment. The patients were followed-up for 6 months after clinical cure to look for recurrence. In the IMQ group (group A), the overall complete cure rate was 91.8% (34 of 37), 22 of the 37 patients cleared by the end of 6 weeks and 12 more patients cleared by the end of 12 weeks, while the remaining three patients (8.1%) did not clear even after 16 weeks. Whereas, in the cryotherapy group, all 37 patients achieved complete cure, 26 of 37 (70.27%) patients cleared after 3 weeks, and the remaining 11 (29.72%) cleared by the end of 6 weeks. No statistically significant difference was found between the overall complete cure rate in both groups at the end of maximum treatment period (16 weeks). Pain, bullae formation, pigmentary changes, and superficial scarring were more significantly common in the cryotherapy group compared with the IMQ group. Imiqimod 5% cream seems to be slow acting but an effective agent for the treatment of MC in children. IMQ appears to be practically painless and more cosmetically accepted treatment when compared with cryotherapy, and may be the preferred treatment of MC in children especially with numerous small lesions. Cryotherapy has the advantage of being rapidly effective, and is less expensive than IMQ and may be the preferred treatment for large solitary or few lesions.
==========================================================
28.) Topical 0.3% and 0.5% podophyllotoxin cream for self-treatment of molluscum contagiosum in males. A placebo-controlled, double-blind study.
===========================================================
Dermatology. 1994;189(1):65-8.
Syed TA1, Lundin S, Ahmad M.
Author information
1
Department of Clinical Physiology, Malmö University Hospital, University of Lund, Sweden.
Abstract
BACKGROUND:
Molluscum contagiosum is generally a self-limiting benign skin disease that affects mostly children and young adults.
OBJECTIVE:
The purpose of this multicenter, double-blind, placebo-controlled study was to compare the clinical efficacy and tolerance of 0.3% and 0.5% podophyllotoxin in a hydrophilic cream base to cure molluscum contagiosum in Asian males.
METHODS:
Preselected patients (n = 150), age range 10-26 years (mean: 15.4), harboring 1,125 lesions (mean: 7.5), with size ranging from 2 to 8 mm in diameter (mean spot size 3.2 mm) and biopsy-proven diagnosis of molluscum contagiosum, were randomly allocated to three parallel groups. Twenty-four (16%) patients had atopic dermatitis. Patients self-administered placebo, 0.3% or 0.5% podophyllotoxin cream, twice daily for 3 consecutive days, and if total elimination was not achieved with one trial (6 topical applications), the same treatment was extended to 3 more weeks (24 topical applications in 4 weeks). The duration of the study was 12 weeks with 6 months (on monthly basis) follow-up. By the end of the treatment 80 patients (52, 92 and 16% patients in the 0.3%, 0.5% and the placebo groups, respectively) were evaluated as completely cured. During the treatment 92 patients (61.3%) did not complain of any allergic or localized adverse symptoms. Tolerable moderate to mild frequent side effects were pruritus (20.6%) and erythema (18%), with no dropouts. No recurrence was seen after 9 months of follow-up. Response to the trial medications appeared to be directly proportional to the concentration of podophyllotoxin (p < 0.001). Self-medication was well accepted by all the patients. It was concluded that the 0.5% podophyllotoxin cream preparation was more efficacious than the 0.3% incorporation (p < 0.001) and can be considered a safe, home-based first line of therapy to cure molluscum contagiosum.
==========================================================
29.) Comparative study of 5% and 2.5% potassium hydroxide solution for molluscum contagiosum in children.
===========================================================
Cutan Ocul Toxicol. 2014 Mar;33(1):54-9. doi: 10.3109/15569527.2013.796479. Epub 2013 May 29.
Uçmak D1, Akkurt MZ, Kacar SD, Sula B, Arica M.
Author information
1
Department of Dermatology, Dicle University , Diyarbakir , Turkey and.
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is a pediatric viral infection that is fairly contagious. Although various treatment methods are available, the presence of facial lesions limits options of therapy.
AIM:
We aimed to test an alternative treatment consisting of application of two different concentrations of potassium hydroxide (of KOH 5% solution and of KOH 2.5% solution) aqueous solution.
METHODS:
In this study we evaluated the effectiveness and side-effects of daily applications of potassium hydroxide (KOH) aqueous solution at 2.5% and 5% concentrations, twice daily in 29 children with MC. Out of a total of 29 patients with molluscum contagiosum included in the study, 13 patients in the 2.5% KOH group and 12 patients in the KOH 5% group completed the study. Families were instructed to apply potassium hydroxide twice a day. The assessment of response and side-effects were performed on days 0, 15, 30, 45 and 60 (visits were numbered 1, 2, 3, 4 and 5, respectively) and one month after.
RESULTS:
We had a total of 11 (44%) patients who completely recovered after the fifth visit. While eight (66.7%) of these 11 patients were in the 5% treatment group, three (23.1%) patients were in the 2.5% treatment group, and there was a statistically meaningful difference (p < 0.047). Patients with fewer lesions remitted better (p < 0.05). When number of lesions were taken into consideration, difference between the two treatment groups appeared after the fourth visit (p < 0.001). There were no statistical differences between the two groups with respect to side-effects (p = 0.682).
CONCLUSIONS:
Potassium hydroxide solution at a concentration of 5% was more effective than 2.5% in our patients. The treatment was well-tolerated on the face with the advantage of administration of lower concentrations. This study suggests potassium hydroxide may be a more preferable mode of treatment for molluscum contagiosum lesions on the face.
==========================================================
30.) Combination topical treatment of molluscum contagiosum with cantharidin and imiquimod 5% in children: a case series of 16 patients.
==========================================================
Australas J Dermatol. 2004 May;45(2):100-2.
Ross GL1, Orchard DC.
Author information
1
Dermatology Department, Royal Children's Hospital, Flemington Road, Parkville, Melbourne, Victoria 5052, Australia.
Abstract
The objective of this study was to assess the efficacy and tolerability of combination therapy for molluscum contagiosum (MC) with topical cantharidin and imiquimod 5%. A prospective case series of 16 paediatric patients with a mean age of 4.8 years had cantharidin applied to lesions by a dermatologist, followed by home treatment with imiquimod 5% cream nightly for an average of 5 weeks. This regimen resulted in >90% of lesions clearing in 12 patients, with half of these being totally clear. Two patients had 80-90% of lesions resolve. Two patients had 30-50% clearance of lesions at the end of the treatment period. One patient found the cantharidin reaction too strong. The mean number of imiquimod 250 mg sachets used was 4.25. In conclusion, this study suggests that combination therapy using cantharidin and imiquimod for treatment of MC in children is effective and well tolerated.
==========================================================
31.) Topical treatment of molluscum contagiosum with imiquimod 5% cream in Turkish children.
==========================================================
Pediatr Int. 2006 Aug;48(4):403-5.
Arican O1.
Author information
1
Department of Dermatology, Medical Faculty, Kahramanmaras Sutcuimam University, Kahramanmaras, Turkey. ozerari@gmail.com
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is caused by a poxvirus which produces cutaneous lesions appearing as small, firm, umbilicated papules. Lesions of MC are most commonly seen in young children. Transmission is through viral particles, which remain on surfaces, autoinoculation, or from contact with open lesions. There are many options for treatment of MC and these may be broadly subdivided into destructive, immunological and antiviral therapies. An alternative treatment would be desirable in pediatric patients. Imiquimod (IQ) is a member of immune response modifiers.
METHODS:
Here, the results of 12 Turkish pediatric patients with MC who used IQ 5% cream (aged between 3-13 years; six boys, six girls) are given. The cream was applied by the mothers in the evening, three times per week every other day up to 16 weeks.
RESULTS:
One of the patients gave up the treatment because of Influenza-like symptoms, and two of them because of the progress in the lesions continued. In seven of the remaining nine patients, total recovery was achieved. Local side-effects in patients were well tolerated.
CONCLUSION:
When all the patients affected with MC who exclusively used IQ 5% cream as mentioned in the literature were studied, 35 of 83 patients (42.2%) had complete clearance. These have differences in the form and duration of application. IQ 5% cream can be preferred in the treatment of children with MC because of its applicability at home, easy application and good tolerability. However, different application methods and suitable treatment methods should be determined.
==========================================================
32.) Treatment of molluscum contagiosum with cantharidin: a practical approach.
==========================================================
Pediatr Ann. 2010 Mar;39(3):124-8, 130. doi: 10.3928/00904481-20100223-03.
Mathes EF1, Frieden IJ.
Author information
1
Department of Dermatology, University of California, San Francisco, USA. mathese@derm.ucsf.edu
Abstract
Molluscum contagiosum is very common. In this article we discuss the use of cantharidin as a treatment option for molluscum contagiosum and give detailed information about distribution sources, how to apply it, and caveats regarding its use.Molluscum contagiosum is a common viral disease of childhood caused by a poxvirus, which presents with small, firm, dome-shaped, umbilicated papules. It is generally benign and self-limited, with spontaneous resolution within 6 months to several years. Watchful waiting can often be an appropriate management strategy; however, some patients either desire or require treatment. Reasons for actively treating molluscum contagiosum may include alleviation of discomfort and itching (particularly in patients where an eczematous eruption - the so-called "molluscum eczema" - is seen in association) or in patients with ongoing atopic dermatitis where more lesions are likely to be present. Other reasons for treatment include limitation of spread to other areas and people, prevention of scarring and superinfection, and elimination of the social stigma of visible lesions. No one treatment is uniformly effective.Treatment options include destructive therapies (curettage, cryotherapy, cantharidin, and keratolytics, among others), immunomodulators (imiquimod, cimetidine, and Candida antigen), and antivirals (cidofovir). In this article we discuss and describe our first-line treatment approach for those molluscum needing treatment - cantharidin.
==========================================================
33.) Treatment of molluscum contagiosum with oral cimetidine: clinical experience in 13 patients.
==========================================================
Pediatr Dermatol. 1996 Jul-Aug;13(4):310-2.
Dohil M1, Prendiville JS.
Author information
1
British Columbia's Children's Hospital, Vancouver, Canada.
Abstract
Our purpose was to determine if oral cimetidine, a histamine-receptor antagonist, might be of benefit in the treatment of extensive molluscum contagiosum in children. We present 13 pediatric patients in whom conventional treatment modalities for molluscum contagiosum were unsuccessful or difficult to apply. They were treated with a two-month course of oral cimetidine 40 mg/kg/day. All but three children who completed treatment experienced clearance of all lesions. These children had no new lesions but had persistence of several lesions. One child did not take the drug and did not clear. No adverse effects were observed. We conclude that oral cimetidine may be of benefit in the management of widespread or facial molluscum contagiosum in immunocompetent children.
Comment in
==========================================================
34.) Treatment of molluscum contagiosum: a brief review and discussion of a case successfully treated with adapelene.
===========================================================
Dermatol Online J. 2007 Jul 13;13(3):15.
Scheinfeld N1.
Author information
1
Columbia University Department of Dermatology, USA.
Abstract
Molluscum contagiosum occur in 2-8 percent of children. This infection is among the most common viral skin infections in children. Although the lesions will resolve spontaneously when puberty, there are several reasons to treat them. The lesions can be cosmetically unappealing. About 10 percent of those with this infection develop a pruritic eczematous eruption. In about 4 percent of children with molluscum, the lesions are numerous and recurrent with no other coexisting immunological problem. Patients who have atopic dermatitis may develop widespread involvement with molluscum. Treatment options include destruction, topical therapy, and oral therapy. Destructive treatment modalities include curettage, cryotherapy, expression or pricking with a sterile needle, electrodesiccation, photodynamic therapy, and laser ablation. Destructive therapy is poorly tolerated in children. Topical medical therapy includes salicylic acid, glycolic acid, tretinoin, tazortene, 5 percent sodium nitrite co-applied daily with 5 percent salicylic acid topical preparations, podofilox, liquefied phenol, tretinoin, cantharidin, and potassium hydroxide. Oral treatment of molluscum includes cimetidine. No therapy is universally effective. I report herein a case of generalized numerous and recurrent molluscum treated with minimal irritation with adapelene.
==========================================================
35.) Interventions for cutaneous molluscum contagiosum.
==========================================================
van der Wouden JC1, van der Sande R, van Suijlekom-Smit LW, Berger M, Butler CC, Koning S.
Author information
1
Department of General Practice, Erasmus MC, University Medical Center, PO Box 1738, Rotterdam, Zuid-Holland, Netherlands, 3000 DR.
Abstract
BACKGROUND:
Molluscum contagiosum is a common skin infection, caused by a pox virus. The infection will usually resolve within months in people with a normal immune system. Many treatments have been used for molluscum contagiosum but a clear evidence base supporting them is lacking.This is an updated version of the original Cochrane Review published in Issue 2, 2006.
OBJECTIVES:
To assess the effects of management strategies (including waiting for natural resolution) for cutaneous, non-genital molluscum contagiosum in otherwise healthy people.
SEARCH STRATEGY:
In June 2009 we updated our searches of the Cochrane Skin Group Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (Issue 2, 2009), MEDLINE, EMBASE, and LILACS. We also searched ongoing trials registers, reference lists, and contacted pharmaceutical companies and experts in the field.
SELECTION CRITERIA:
We investigated randomised controlled trials (RCTs) for the treatment of molluscum contagiosum. We excluded trials on sexually transmitted molluscum contagiosum and in people with lowered immunity (including those with HIV infection).
DATA COLLECTION AND ANALYSIS:
Two authors independently selected studies, assessed methodological quality, and extracted data from selected studies.
MAIN RESULTS:
Eleven studies, with a total number of 495 participants, examined the effects of topical (9 studies), systemic, and homoeopathic interventions (1 study each). Limited evidence was found for the efficacy of sodium nitrite co-applied with salicylic acid compared to salicylic acid alone (risk ratio (RR) 3.50, 95% confidence interval (CI) 1.23 to 9.92); for Australian lemon myrtle oil compared to its vehicle, olive oil (RR 17.88, 95% CI 1.13 to 282.72); and for benzoyl peroxide cream compared to tretinoin (RR 2.20, 95% CI 1.01 to 4.79). No statistically significant differences were found for 10 other comparisons, most of which addressed 2 topical treatments.Study limitations included no blinding (four studies), many dropouts (three studies), and no intention-to-treat analysis; small study sizes may have led to important differences being missed. None of the evaluated treatment options were associated with serious adverse effects.
AUTHORS' CONCLUSIONS:
No single intervention has been shown to be convincingly effective in the treatment of molluscum contagiosum. The update identified six new studies, most of them reporting on interventions not included in the original version. However, the conclusions of the review did not change.
==========================================================
36.) Giant Molluscum Contagiosum in an HIV positive patient.
==========================================================
Int J Infect Dis. 2015 Sep;38:153-5. doi: 10.1016/j.ijid.2015.07.021. Epub 2015 Aug 6.
Pérez-Díaz CE1, Botero-García CA2, Rodríguez MC3, Faccini-Martínez ÁA4, Calixto OJ5, Benítez F5, Mantilla-Florez YF5, Bravo-Ojeda JS6, Espinal A6, Morales-Pertuz C6.
Author information
1
Servicios y Asesorías en Infectología (SAI), Bogotá, Colombia; Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia; Medicine school, Universidad Militar Nueva Granada, Bogotá, Colombia.
2
Medicine school, Universidad Militar Nueva Granada, Bogotá, Colombia.
3
Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia; Dermatology Department, Hospital Militar Central, Bogotá, Colombia.
4
Servicios y Asesorías en Infectología (SAI), Bogotá, Colombia; Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia. Electronic address: afaccini@gmail.com.
5
Servicios y Asesorías en Infectología (SAI), Bogotá, Colombia; Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia.
6
Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia; Internal Medicine department, Hospital Militar Central, Bogotá, Colombia.
Abstract
Molluscum Contagiosum (MC) is a skin infection caused by a double-stranded DNA virus of the family Poxviridae that replicates in the human epidermis, affecting mainly children and young sexually active adults and causing flesh colored papular lesions with central umbilication with an average size of 3-5mm, although atypical lesions that reach great size (Giant Molluscum Contagiosum), 10-15mm, can be seen in almost any immunodeficiency condition. We report the case of a 35 year old male patient with C3 HIV disease with an abdominal pathology associated to skin lesions predominantly in the forehead and scalp that reached sizes over 5mm, diagnosed as Giant Molluscum Contagiosum by skin biopsies.
==========================================================
37.) Giant molluscum contagiosum: an unusual presenting complaint of paediatric HIV disease.
==========================================================
Trop Doct. 2015 Apr;45(2):148-50. doi: 10.1177/0049475514568133. Epub 2015 Jan 18.
Chatterjee S1, Banerjee M2, Bhattacharya S3.
Author information
1
Resident, Department of Paediatrics, Medical College, Kolkata, India sayanchat_82@yahoo.co.in.
2
Resident, Department of Paediatrics, Medical College, Kolkata, India.
3
Associate Professor, Department of Paediatrics Medical College, Kolkata, India.
Abstract
We report a widely disseminated, disfiguring facial molluscum contagiosum (MC) as a presenting complaint in an 11-year-old girl secondary to human immune-deficiency virus infection. A biopsy specimen demonstrated lobulated epidermal growth consisting of keratinocytes with large intracytoplasmic eosinophilic inclusion bodies. The patient was treated with highly active anti-retroviral therapy (HAART). The extent of MC in our patient was remarkable and subsequently improved dramatically after starting HAART. Normally MC does not similarly respond in patients with AIDS.
==========================================================
38.) Generalized molluscum contagiosum in an HIV patient treated with diphencyprone.
==========================================================
J Dermatol Case Rep. 2010 Dec 31;4(4):60-2. doi: 10.3315/jdcr.2010.1059.
Chularojanamontri L1, Tuchinda P, Kulthanan K, Manuskiatti W.
Author information
1
Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand.
Abstract
BACKGROUND:
Diphencyprone is a universal contact immunotherapy. The mechanism of action is based on an induction of the delayed-type hypersensitivity. Diphencyprone has been used in various forms for treatments of recalcitrant and facial warts, and alopecia areata. However, this treatment modality has not been generally used in immunocompromised patients.
MAIN OBSERVATION:
The present report demonstrated the efficacy of diphencyprone immunotherapy on the treatment of generalized molluscum contagiosum in a human immunodeficiency virus (HIV)-infected patient. Minimal and transient side effects including pruritus, postinflammatory hyperpigmentation and irritation were noted.
CONCLUSION:
Diphencyprone contact immunotherapy appears to be a possible alternative treatment of widespread molluscum contagiosum in immunocompromised patients.
==========================================================
39.) Molluscum contagiosum effectively treated with a topical acidified nitrite, nitric oxide liberating cream.
==========================================================
Br J Dermatol. 1999 Dec;141(6):1051-3.
Ormerod AD1, White MI, Shah SA, Benjamin N.
Author information
1
Department of Dermatology, Aberdeen Royal Infirmary, Foresthill, UK. a.d.ormerod@abdn.ac.uk
Abstract
A double-blind, group-sequential clinical trial of acidified nitrite was performed to demonstrate the efficacy of this nitric oxide donor in treating molluscum contagiosum. Subjects received either 5% sodium nitrite co-applied with 5% salicylic acid under occlusion, or identical cream with 5% salicylic acid, omitting sodium nitrite. Active and control treatment groups were well matched for the number and duration of lesions and made a similar number of applications. We found a 75% cure rate in the active treatment group and 21% cure with control treatment (P = 0.01). The mean time to cure was 1.83 months. Staining of the skin and irritation were frequent side-effects but did not prevent successful treatment.
==========================================================
40.) Treatment of molluscum contagiosum with silver nitrate paste.
==========================================================
Pediatr Dermatol. 1999 Sep-Oct;16(5):395-7.
Niizeki K1, Hashimoto K.
Author information
1
Chigasaki Dermatology Clinic, Nanko, Japan.
Abstract
Three hundred eighty-nine consecutive patients with molluscum contagiosum were treated with 40% silver nitrate paste. The cure rate was 97.7% and no scars resulted.
==========================================================
41.) Efficacy of pulsed dyed laser (585 nm) in the treatment of molluscum contagiosum subtype 1.
==========================================================
Southeast Asian J Trop Med Public Health. 2007 Sep;38(5):849-54.
Chatproedprai S1, Suwannakarn K, Wananukul S, Theamboonlers A, Poovorawan Y.
Author information
1
Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
Abstract
Molluscum contagiosum is a common cutaneous disease that may be difficult to treat when there are multiple lesions; especially in children. This study was conducted to determine the efficacy of pulsed dye laser (585 nm) in the treatment of molluscum contagiosum in 20 children. In the treated group, 70.5% of lesions healed after the first treatment; the remaining 10.6% after the second treatment (2 weeks later). The overall cure rate was significantly different from the control group (p< 0.01). The therapy was also well tolerated. Only mild transient hypopigmentation and erythema were observed. None encountered infectious events. In conclusion, pulsed dye laser is a good alternative treatment for molluscum contagiosum due to high efficacy and mild transient side effects.
==========================================================
42.) Oral griseofulvin therapy in molluscum contagiosum.
==========================================================
Indian J Dermatol. 1987 Oct;32(4):104-6.
Mukul, Meena HS, Gupta S.
==========================================================
43.) [Molluscum contagiosum treated by topical using 10% tincture of iodine].
==========================================================
[Article in Chinese]
==========================================================
REFRENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
=============================================================
1.) [Molluscum contagiosum--a common but poorly understood "childhood disease" and sexually transmitted illness].
2.) Immune evasion strategies of molluscum contagiosum virus.
3.) Identification and typing of molluscum contagiosum virus in clinical specimens by polymerase chain reaction.
4.) Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study.
5.) [THE DIFFERENT PRESENTATIONS OF PERIOCULAR MOLLUSCUM CONTAGIOSUM].
6.) Molluscum contagiosum and associations with atopic eczema in children: a retrospective longitudinal study in primary care.
7.) Clinical and Demographic Characteristics of Patients with Molluscum Contagiosum Treated at the University Dermatology Clinic Maribor in a 5-year period.
8.) Molluscum contagiosum: to treat or not to treat? Experience with 170 children in an outpatient clinic setting in the northeastern United States.
9.) Successful treatment of molluscum contagiosum with intralesional immunotherapy by measles, mumps, and rubella vaccine: a report of two cases.
10.) Intralesional immunotherapy with Candida antigen for the treatment of molluscum contagiosum in children.
11.) Congenital molluscum contagiosum: report of four cases and review of the literature.
12.) Molluscum contagiosum virus infection.
13.) Extensive molluscum contagiosum virus infection in a young adult receiving fingolimod.
14.) Rapid detection and typing of Molluscum contagiosum virus by FRET-based real-time PCR.
15.) Seroprevalence of Molluscum contagiosum virus in German and UK populations.
16.) Disparate antiviral responses in Molluscum contagiosum virus-induced skin lesions.
17.) Close relationship between equine and human molluscum contagiosum virus demonstrated by in situ hybridisation.
18.) Topical 20% KOH--an effective therapeutic modality for moluscum contagiosum in children.
19.) Treatment of pediatric molluscum contagiosum with 10% potassium hydroxide solution.
20.) Topical salicylic acid gel as a treatment for molluscum contagiosum in children.
21.) Essential oil of Australian lemon myrtle (Backhousia citriodora) in the treatment of molluscum contagiosum in children.
22.) Modified curettage technique for molluscum contagiosum.
23.) Curettage treatment for molluscum contagiosum: a follow-up survey study.
24.) An open, comparative study of 10% potassium hydroxide solution versus salicylic and lactic acid combination in the treatment of molluscum contagiosum in children.
25.) Comparative study of 5 % potassium hydroxide solution versus 0.05% tretinoin cream for Molluscum Contagiosum in children.
26.) A comparative study of 10% KOH solution and 5% imiquimod cream for the treatment of Molluscum contagiosum in the pediatric age group.
27.) Comparative study on the efficacy, safety, and acceptability of imiquimod 5% cream versus cryotherapy for molluscum contagiosum in children.
28.) Topical 0.3% and 0.5% podophyllotoxin cream for self-treatment of molluscum contagiosum in males. A placebo-controlled, double-blind study.
29.) Comparative study of 5% and 2.5% potassium hydroxide solution for molluscum contagiosum in children.
30.) Combination topical treatment of molluscum contagiosum with cantharidin and imiquimod 5% in children: a case series of 16 patients.
31.) Topical treatment of molluscum contagiosum with imiquimod 5% cream in Turkish children.
32.) Treatment of molluscum contagiosum with cantharidin: a practical approach.
33.) Treatment of molluscum contagiosum with oral cimetidine: clinical experience in 13 patients.
34.) Treatment of molluscum contagiosum: a brief review and discussion of a case successfully treated with adapelene.
35.) Interventions for cutaneous molluscum contagiosum.
36.) Giant Molluscum Contagiosum in an HIV positive patient.
37.) Giant molluscum contagiosum: an unusual presenting complaint of paediatric HIV disease.
38.) Generalized molluscum contagiosum in an HIV patient treated with diphencyprone.
39.) Molluscum contagiosum effectively treated with a topical acidified nitrite, nitric oxide liberating cream.
40.) Treatment of molluscum contagiosum with silver nitrate paste.
41.) Efficacy of pulsed dyed laser (585 nm) in the treatment of molluscum contagiosum subtype 1.
42.) Oral griseofulvin therapy in molluscum contagiosum.
43.) [Molluscum contagiosum treated by topical using 10% tincture of iodine].
44.) Topical and intralesional cidofovir: a review of pharmacology and therapeutic effects. =======================================================
=======================================================
1.) [Molluscum contagiosum--a common but poorly understood "childhood disease" and sexually transmitted illness].
=======================================================
Med Monatsschr Pharm. 2013 Aug;36(8):282-90.
[Article in German]
Stock I1.
Author information
1
Institut für Medizinische Mikrobiologie, Immunologie und Parasitologie, Abteilung Pharmazeutische Mikrobiologie, Universität Bonn, Bonn. Ingo_Stock@web.de
Abstract
Molluscum contagiosum is a viral disease of the skin characterized by discrete, multiple, flesh-colored papules. It is caused by a highly infectious, enveloped deoxyribonucleic acid virus, called molluscum contagiosum virus (MCV). Molluscum contagiosum is very common in children, sexually active adults and immunocompromised patients, especially those who are infected with the human immunodeficiency virus. MCV transmission usually takes place through direct skin-to-skin contact. Infections in childhood are often linked to swimming-pool attendance. Adults are infected usually through sexual contact. An intimate skin-to-skin contact is sufficient for transmission of the virus. In immunocompetent adults, the warts remain in the genital area and adjacent regions of the skin. In children and patients with immunocompromised conditions, however, various regions of the body are usually affected. Therapy of molluscum contagiosum should be undertaken in an individualized manner, a specific treatment does not exist. For the treatment, physical methods such as curettage and cryotherapy, topic acids (e. g., acetic acid) and alkalis (e. g., potassium hydroxide), some other topical agents such as cantharidin and imiquimod, as well as several systemic agents the pharmacological treatments is, however, sparse. Effective prevention is problematic due to the high infectivity of the virus. A vaccine is not available.
==========================================================
2.) Immune evasion strategies of molluscum contagiosum virus.
==========================================================
Adv Virus Res. 2015;92:201-52. doi: 10.1016/bs.aivir.2014.11.004. Epub 2015 Jan 13.
Shisler JL1.
Author information
1
Department of Microbiology, College of Medicine, University of Illinois, Urbana, Illinois, USA. Electronic address: jshisler@illinois.edu.
Abstract
Molluscum contagiosum virus (MCV) is the causative agent of molluscum contagiosum (MC), the third most common viral skin infection in children, and one of the five most prevalent skin diseases worldwide. No FDA-approved treatments, vaccines, or commercially available rapid diagnostics for MCV are available. This review discusses several aspects of this medically important virus including: physical properties of MCV, MCV pathogenesis, MCV replication, and immune responses to MCV infection. Sequencing of the MCV genome revealed novel immune evasion molecules which are highlighted here. Special attention is given to the MCV MC159 and MC160 proteins. These proteins are FLIPs with homologs in gamma herpesviruses and in the cell. They are of great interest because each protein regulates apoptosis, NF-κB, and IRF3. However, the mechanism that each protein uses to impart its effects is different. It is important to elucidate how MCV inhibits immune responses; this knowledge contributes to our understanding of viral pathogenesis and also provides new insights into how the immune system neutralizes virus infections.
==========================================================
3.) Identification and typing of molluscum contagiosum virus in clinical specimens by polymerase chain reaction.
==========================================================
J Med Virol. 1997 Nov;53(3):205-11.
Thompson CH1.
Author information
1
Department of Infectious Diseases, Faculty of Medicine, University of Sydney, NSW, Australia.
Abstract
A polymerase chain reaction (PCR) which enables the detection of molluscum contagiosum virus (MCV) genomes in either fresh or formalin-fixed clinical specimens is described. The primers used were designed to amplify a 167 bp region of the 3.8 kbp HindIII fragment K of the MCV 1 genome. The ability of this PCR to detect three common MCV types (1, 1v and 2) in clinical specimens was confirmed using frozen extracts from 75 molluscum lesions, and digests of single sections of 11 formalin-fixed, paraffin-embedded lesions; all of which had been previously typed by Southern hybridisation. In addition, 2 specimens previously negative by hybridisation were shown to be positive for MCV DNA by PCR. Confirmation of the identity of the PCR products and distinction between the two major MCV types (MCV 1/1v versus MCV 2) was achieved by comparison of the results of cleavage with the restriction endonucleases Hhal and Sacl. Sequencing of the PCR products revealed complete homology between MCV 1 and 1v, but minor nucleotide variations between MCV 1/1v and MCV 2 were identified. As well as providing a highly sensitive means of diagnosis, the technique may also prove useful for investigations into the pathogenesis, epidemiology and natural history of molluscum contagiosum infection.
==========================================================
4.) Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study.
===========================================================
Lancet Infect Dis. 2015 Feb;15(2):190-5. doi: 10.1016/S1473-3099(14)71053-9. Epub 2014 Dec 23.
Olsen JR1, Gallacher J2, Finlay AY3, Piguet V3, Francis NA2.
Author information
1
Cochrane Institute of Primary Care and Public Health, Cardiff University, Cardiff, Wales, UK. Electronic address: olsenjr@cardiff.ac.uk.
2
Cochrane Institute of Primary Care and Public Health, Cardiff University, Cardiff, Wales, UK.
3
Department of Dermatology and Academic Wound Healing, Institute of Infection and Immunity, Cardiff University and University Hospital of Wales, Cardiff, Wales, UK.
Abstract
BACKGROUND:
Molluscum contagiosum is one of the 50 most prevalent diseases worldwide, but scarce epidemiological data exist for childhood molluscum contagiosum. We aimed to describe the time to resolution, transmission to household child contacts, and effect on quality of life of molluscum contagiosum in children in the UK.
METHODS:
Between Jan 1, and Oct 31, 2013, we recruited 306 children with molluscum contagiosum aged between 4 and 15 years in the UK either by referral by general practitioner or self-referral (with diagnosis made by parents by use of the validated Molluscum Contagiosum Diagnostic Tool for Parents [MCDTP]). All participants were asked to complete a questionnaire at recruitment about participant characteristics, transmission, and quality of life. We measured quality of life with the Children's Dermatology Life Quality Index (CDLQI). Participants were prospectively followed up every month to check on their recovery from molluscum contagiosum and transmission to other children in the same household, until the child's lesions were no longer visible.
FINDINGS:
The mean time to resolution was 13·3 months (SD 8·2). 80 (30%) of 269 cases had not resolved by 18 months; 36 (13%) had not resolved by 24 months. We recorded transmission to other children in the household in 102 (41%) of 250 cases. Molluscum contagiosum had a small effect on quality of life for most participants, although 33 (11%) of 301 participants had a very severe effect on quality of life (CDLQI score >13). A greater number of lesions was associated with a greater effect on quality of life (H=55·8, p<0·0001).
INTERPRETATION:
One in ten children with molluscum contagiosum is likely to have a substantial effect on their quality of life and therefore treatment should be considered for some children, especially those with many lesions or who have been identified as having a severe effect on quality of life. Patients with molluscum contagiosum and their parents need to be given accurate information about the expected natural history of the disorder. Our data provide the most reliable estimates of the expected time to resolution so far and can be used to help set realistic expectations.
FUNDING:
Wales School of Primary Care Research (WSPCR) and Cardiff University.
==========================================================
5.) [THE DIFFERENT PRESENTATIONS OF PERIOCULAR MOLLUSCUM CONTAGIOSUM].
===========================================================
Harefuah. 2015 Nov;154(11):703-7, 742.
[Article in Hebrew]
Zloto O, Rosner M.
Abstract
INTRODUCTION:
Periocular molluscum contagiosum nodules typically appear in a classical presentation. However, the presentation can be different. This makes the diagnosis and the decision on treatment difficult.
AIM:
To report different clinical presentations of periocular molluscum contagiosum and to examine their epidemiological, clinical and histopathological features.
METHODS:
For all patients who were diagnosed with periocular molluscum contagiosum during the years 1995-2014, the following data was extracted from the patients' files: gender, age at the time of diagnosis, location of the lesion, number and dimensions of lesions, clinical presentation, histopathological features, suspected clinical diagnosis before histopathological diagnosis and treatment. A classification according to different presentations was suggested and the epidemiological, clinical and histopathological features of each presentation were examined.
RESULTS:
Molluscum contagiosum was diagnosed in 30 patients: 10 males (33.33%) and 20 females (66.66%). The mean age of diagnosis was 19.3 years old, one patient was immunosuppressive and 29 patients were immunocompetent. Six different clinical presentations were seen: Typical, umbilicated dome shaped lesion (19 cases), big lesion (4 cases), conglomerated lesions (4 cases), erythematous lesion (1 case), inflamed lesion (1 case), and pedunculated lesion (1 case). In all cases the diagnosis was confirmed by histopathological examination and the treatment was surgical excision.
CONCLUSION:
According to this case series of periocular molluscum contagiosum, which is one of the largest published thus far in the ophthalmic literature, six distinct different clinical presentations are suggested. These lesions should be suspected not just in children and in immunosuppressive adult patients but also in immunocompetent patients of all ages.
==========================================================
6.) Molluscum contagiosum and associations with atopic eczema in children: a retrospective longitudinal study in primary care.
==========================================================
Br J Gen Pract. 2016 Jan;66(642):e53-8. doi: 10.3399/bjgp15X688093. Epub 2015 Dec 6.
Olsen JR1, Piguet V2, Gallacher J3, Francis NA4.
Author information
1
Institute of Health and Wellbeing, College of Medical Veterinary and Life Sciences, University of Glasgow, Glasgow.
2
Professor and head of Department of Dermatology and Academic Wound Healing, Division of Infection and Immunity, School of Medicine, Cardiff University, Cardiff.
3
Department of Psychiatry, Medical Sciences Division, University of Oxford, Oxford.
4
Cochrane Institute of Primary Care and Public Health, School of Medicine, Cardiff University, Cardiff.
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is a common skin condition in children. Consultation rates and current management in primary care, and how these have changed over time, are poorly described. An association between the presence of atopic eczema (AE) and MC has been shown, but the subsequent risk of developing MC in children with a diagnosis of AE is not known.
AIM:
To describe the consultation rate and management of MC in general practice in the UK over time, and test the hypothesis that a history of AE increases the risk of developing MC in childhood.
DESIGN AND SETTING:
Two studies are reported: a retrospective longitudinal study of MC cases and an age-sex matched case-cohort study of AE cases, both datasets being held in the UK Clinical Practice Research Datalink from 2004 to 2013.
METHOD:
Data of all recorded MC and AE primary care consultations for children aged 0 to 14 years were collected and two main analyses were conducted using these data: a retrospective longitudinal analysis and an age-sex matched case-cohort analysis.
RESULTS:
The rate of MC consultations in primary care for children aged 0 to 14 years is 9.5 per 1000 (95% CI = 9.4 to 9.6). The greatest rate of consultations for both sexes is in children aged 1-4 years and 5-9 years (13.1 to 13.0 (males) and 13.0 to 13.9 (females) per 1000 respectively). Consultation rates for MC have declined by 50% from 2004 to 2013. Children were found to be more likely to have an MC consultation if they had previously consulted a GP with AE (OR 1.13; 95% CI = 1.11 to 1.16; P<0.005).
CONCLUSION:
Consultations for MC in primary care are common, especially in 1-9-year-olds, but they declined significantly during the decade under study. A primary care diagnosis of AE is associated with an increased risk of a subsequent primary care diagnosis of MC.
==========================================================
7.) Clinical and Demographic Characteristics of Patients with Molluscum Contagiosum Treated at the University Dermatology Clinic Maribor in a 5-year period.
==========================================================
Acta Dermatovenerol Croat. 2016 Jun;24(2):130-6.
Trčko K1, Poljak M, Križmarić M, Miljković J.
Author information
1
Katarina Trčko, MD, Department of Dermatovenereology, University Clinical Centre Maribor, Ljubljanska 5, 2000 Maribor, Slovenia; katarina.trcko@gmail.com.
Abstract
Molluscum contagiosum virus (MCV) is a common skin pathogen in both adults and children. In this prospective study, we clinically evaluated consecutive patients with molluscum contagiosum (MC) who had been examined during a 5-year period at the second-largest dermatology clinic in Slovenia and described their main demographic and clinical characteristics, concomitant diseases, and treatment success. The study included 188 patients, of which 121 (64%) were men and 67 (36%) were women. A total of 135 (72%) patients were adults, with lesions that were most commonly located in the anogenital region (98%) and were probably sexually acquired. Two adult patients were diagnosed with concurrent human immunodeficiency virus (HIV) infection. Fifty-three (28%) patients were children with a mean age of 5.7 years, most commonly presenting with lesions on the torso and extremities (85%). In adults, the infection most commonly occurred in male patients, while in children it was slightly more common in female patients. At presentation, 58% of patients had more than 5 MC lesions. A total of 30% of the included children had concomitant atopic dermatitis. We did not observe an increased occurrence of MCV infection in patients with atopic dermatitis. All patients were treated with curettage of the lesions. The cure rate at the first follow-up visit after 2 months was relatively high (63%), and recurrences were not associated with the number or site of lesions at presentation or with concomitant atopic dermatitis.
==========================================================
8.) Molluscum contagiosum: to treat or not to treat? Experience with 170 children in an outpatient clinic setting in the northeastern United States.
==========================================================
Pediatr Dermatol. 2015 May-Jun;32(3):353-7. doi: 10.1111/pde.12504. Epub 2015 Jan 30.
Basdag H1, Rainer BM1, Cohen BA1.
Author information
1
Division of Pediatric Dermatology, Departments of Pediatrics and Dermatology, Johns Hopkins University School of Medicine, Baltimore, Maryland.
Abstract
Despite the high prevalence of molluscum contagiosum (MC) in children, epidemiologic data on this common self-limited viral infection is limited. In this report we review our experience with the demographic characteristics, clinical characteristics, management, and time to resolution of MC in 170 children. A retrospective medical chart review and telephone survey were conducted on children younger than 16 years of age evaluated for MC in the Division of Pediatric Dermatology at the Johns Hopkins Children's Center, Baltimore, Maryland, from January 1, 2008, to December 31, 2011. Of 170 children with MC, 51.8% were female and 77.1% were Caucasian. The median age at diagnosis was 5 years and 46.5% had a history of atopic dermatitis (AD). Children with AD had significantly more MC lesions than those without (p < 0.05); 72.9% of children did not receive any treatment. MC lesions completely cleared within 12 months in 45.6% of treated and 48.4% of untreated children and within 18 months in 69.5% of treated and 72.6% of untreated children. Treatment (if any), sex, race, diagnosing physician, number of lesions at diagnosis, number of anatomic locations, or history of AD did not predict time to resolution of MC lesions. MC lesions completely resolved in approximately 50% of children within 12 months and in 70% within 18 months. Treatment did not shorten the time to resolution.
==========================================================
9.) Successful treatment of molluscum contagiosum with intralesional immunotherapy by measles, mumps, and rubella vaccine: a report of two cases.
==========================================================
Dermatol Ther. 2014 Nov-Dec;27(6):373-6. doi: 10.1111/dth.12158. Epub 2014 Jul 22.
Na CH1, Kim DJ, Kim MS, Kim JK, Shin BS.
Author information
1
Department of Dermatology, Chosun University Medical School, Gwangju, Korea.
Abstract
Molluscum contagiosum (MC) is a common viral infection of the skin and mucous membrane that often affects young children. Generally, physical removal by surgical curettage is commonly used for the treatment of MC, but the pain during the treatment is a major problem. Thus immunotherapy using various antigens has been introduced recently. Here we present two cases of MC that improved with measles, mumps, and rubella (MMR) vaccine intralesional injection. On the ground of our knowledge, they were the first cases of successful MMR intralesional injection in this disease entity.
==========================================================
10.) Intralesional immunotherapy with Candida antigen for the treatment of molluscum contagiosum in children.
===========================================================
Pediatr Dermatol. 2011 May-Jun;28(3):254-8. doi: 10.1111/j.1525-1470.2011.01492.x.
Enns LL1, Evans MS.
Author information
1
University of Arkansas for Medical Sciences and Arkansas Children's Hospital, USA. lindsayenns@gmail.com
Abstract
Intralesional injection of Candida and other antigens is an established and useful therapy for warts; a cutaneous immune response can induce improvement and or clearance of warts, often with response in anatomically distinct lesions other than those injected. Molluscum contagiosum virus is a common cutaneous infection seen primarily in pediatric dermatology clinics. Treatment is often unsatisfactory, painful, and time consuming. A retrospective chart review was conducted to examine the efficacy of intralesional injection of Candida antigen into a maximum of three individual molluscum lesions. Twenty-nine patients were treated with this therapy; 55% had complete resolution. In addition, 37.9% experienced partial resolution, yielding an overall response rate of 93%. Only two patients failed to respond (6.9%). In addition, only four patients reported a single adverse effect of pain with injection. No other adverse effects were reported or noted clinically. Scarring was absent. No recurrences were reported at the time of publication. This report establishes the efficacy of intralesional injection of Candida for
==========================================================
11.) Congenital molluscum contagiosum: report of four cases and review of the literature.
==========================================================
Pediatr Dermatol. 2008 Sep-Oct;25(5):553-6. doi: 10.1111/j.1525-1470.2008.00730.x.
Connell CO1, Oranje A, Van Gysel D, Silverberg NB.
Author information
1
Department of Dermatology, St. Luke's-Roosevelt Hospital Center, New York, New York 10025, USA.
Abstract
Molluscum contagiosum is a viral infection of the skin and mucous membranes that is caused by infection with the molluscum contagiosum virus. Molluscum contagiosum can be acquired from skin to skin contact which may be during play, in a swimming pool, or through sexual contact. Sexually acquired molluscum is rare in younger children, but becomes quite common during adolescence and young adulthood, after the sexual debut. It has been long known that the human papillomavirus, which causes genital warts, i.e., condyloma accuminatum, can be vertically transmitted through an infected genital tract. Children may not manifest condyloma lesions for a few years. The entity of congenital molluscum has been debated in the literature and only three cases of suspected congenital molluscum have been reported. We report on four more infants with congenital molluscum, two children with congenital lesions, and two children with onset of lesions at 6 weeks of age. Two children had single cutaneous lesions on the extremities and two had lesions of the scalp consistent with the site of cervical pressure. Congenital molluscum appears to be a more common entity than previously reported. Vertical transmission of molluscum should be considered for all infantile cases of molluscum.
==========================================================
12.) Molluscum contagiosum virus infection.
==========================================================
Chen X1, Anstey AV, Bugert JJ.
Author information
1
Department of Dermatology, Ruijin Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China.
Abstract
Molluscum contagiosum virus is an important human skin pathogen: it can cause disfigurement and suffering in children, in adults it is less common and often sexually transmitted. Extensive and persistent skin infection with the virus can indicate underlying immunodeficiency. Traditional ablative therapies have not been compared directly with newer immune-modulating and specific antiviral therapies. Advances in research raise the prospect of new approaches to treatment informed by the biology of the virus; in human skin, the infection is localised in the epidermal layers, where it induces a typical, complex hyperproliferative lesion with an abundance of virus particles but a conspicuous absence of immune effectors. Functional studies of the viral genome have revealed effects on cellular pathways involved in the cell cycle, innate immunity, inflammation, and cell death. Extensive lesions caused by molluscum contagiosum can occur in patients with DOCK8 deficiency-a genetic disorder affecting migration of dendritic and specialised T cells in skin. Sudden disappearance of lesions is the consequence of a vigorous immune response in healthy people. Further study of the unique features of infection with molluscum contagiosum virus could give fundamental insight into the nature of skin immunity.
==========================================================
13.) Extensive molluscum contagiosum virus infection in a young adult receiving fingolimod.
==========================================================
Mult Scler. 2016 Jun;22(7):969-71. doi: 10.1177/1352458516629560. Epub 2016 Feb 9.
Behle V1, Wobser M2, Goebeler M2, Stoevesandt J2.
Author information
1
Department of Dermatology, Venerology and Allergology, University Hospital of Würzburg, Würzburg, Germany Behle_V@ukw.de.
2
Department of Dermatology, Venerology and Allergology, University Hospital of Würzburg, Würzburg, Germany.
Abstract
Fingolimod-related viral infections have been described on several occasions since its introduction in 2010. We hereby add a report on an otherwise immunocompetent, 18-year old Caucasian man with relapsing-remitting multiple sclerosis who developed a protracted and extensive molluscum contagiosum (MC) virus infection shortly after being started on fingolimod. Wide-spread cutaneous MC infections in adult patients are considered indicative of underlying immunosuppression. Neurologists prescribing fingolimod ought to be aware of a possibly increased risk of MC, but also need to know about its relative benignity, lack of extra-cutaneous complications, and adequate treatment options.
==========================================================
14.) Rapid detection and typing of Molluscum contagiosum virus by FRET-based real-time PCR.
==========================================================
J Virol Methods. 2013 Feb;187(2):431-4. doi: 10.1016/j.jviromet.2012.11.008. Epub 2012 Nov 20.
Hošnjak L1, Kocjan BJ, Kušar B, Seme K, Poljak M.
Author information
1
Institute of Microbiology and Immunology, Faculty of Medicine, University of Ljubljana, Ljubljana, Slovenia.
Abstract
A fluorescence resonance energy transfer (FRET)-based real-time PCR (RT-PCR) was developed for very sensitive and specific detection of Molluscum contagiosum virus (MCV), as well as reliable differentiation of the two MCV subtype genetic lineages, MCV1 and MCV2, in a single reaction. The assay employs modified primers specific for the viral MC021L gene and uses two novel FRET hybridization probes to detect polymorphisms specific for each of the two subtypes. The sensitivity of the assay at a 95% detection level for both MCV subtypes was 3.3 DNA copies/reaction and the dynamic range was nine orders of magnitude, discriminating 10-10(9) viral genome equivalents/reaction. Post-amplification probe-specific dissociation analysis differentiated the two viral subtypes reliably in all tested concentrations. Testing of 43 tissue specimens clinically diagnosed as MCV lesions showed complete agreement with the results obtained with previously described MCV specific MC080R Taqman RT-PCR and MC021L whole gene sequencing. The novel assay is simple, robust and easy to perform, and may be of great value for clinical and epidemiological studies of MCV infections and related conditions.
==========================================================
15.) Seroprevalence of Molluscum contagiosum virus in German and UK populations.
==========================================================
PLoS One. 2014 Feb 18;9(2):e88734. doi: 10.1371/journal.pone.0088734. eCollection 2014.
Sherwani S1, Farleigh L1, Agarwal N2, Loveless S3, Robertson N3, Hadaschik E4, Schnitzler P5, Bugert JJ1.
Author information
1
Cardiff University School of Medicine, Institute of Infection and Immunity/Medical Microbiology, Cardiff, United Kingdom.
2
Dr P N Behl Skin Institute and School of Dermatology, New Delhi, India.
3
Cardiff University Medical School, Institute of Psychological Medicine and Clinical Neuroscience, Cardiff, United Kingdom.
4
Universität Heidelberg, Hautklinik, Heidelberg, Germany.
5
Universität Heidelberg, Dept.of Infectious Diseases, Heidelberg, Germany.
Abstract
Molluscum contagiosum virus (MCV) is a significant but underreported skin pathogen for children and adults. Seroprevalence studies can help establish burden of disease. Enzyme linked immunosorbent assay (ELISA) based studies have been published for Australian and Japanese populations and the results indicate seroprevalences between 6 and 22 percent in healthy individuals, respectively. To investigate seroprevalence in Europe, we have developed a recombinant ELISA using a truncated MCV virion surface protein MC084 (V123-R230) expressed in E. coli. The ELISA was found to be sensitive and specific, with low inter- and intra-assay variability. Sera from 289 German adults and children aged 0-40 years (median age 21 years) were analysed for antibodies against MC084 by direct binding ELISA. The overall seropositivity rate was found to be 14.8%. The seropositivity rate was low in children below the age of one (4.5%), peaked in children aged 2-10 years (25%), and fell again in older populations (11-40 years; 12.5%). Ten out of 33 healthy UK individuals (30.3%; median age 27 years) had detectable MC084 antibodies. MCV seroconversion was more common in dermatological and autoimmune disorders, than in immunocompromised patients or in patients with multiple sclerosis. Overall MCV seroprevalence is 2.1 fold higher in females than in males in a UK serum collection. German seroprevalences determined in the MC084 ELISA (14.8%) are at least three times higher than incidence of MC in a comparable Swiss population (4.9%). While results are not strictly comparable, this is lower than Australian seroprevalence in a virion based ELISA (n = 357; 23%; 1999), but higher than the seroprevalence reported in a Japanese study using an N-terminal truncation of MC133 (n = 108, 6%; 2000. We report the first large scale serological survey of MC in Europe (n = 393) and the first MCV ELISA based on viral antigen expressed in E. coli.
==========================================================
16.) Disparate antiviral responses in Molluscum contagiosum virus-induced skin lesions.
==========================================================
J Invest Dermatol. 2011 Feb;131(2):288-90. doi: 10.1038/jid.2010.368.
Swiecki M1, Colonna M.
Author information
1
Department of Pathology and Immunology, Washington University School of Medicine, St Louis, Missouri 63110, USA.
Abstract
Molluscum contagiosum virus (MCV) is a poxvirus that causes tumor-like skin lesions. New evidence indicates that plasmacytoid dendritic cells, type I interferon production, and interferon-induced dendritic cells have prominent roles in anti-MCV responses, and these features characterize the inflammatory response in lesions that will likely undergo spontaneous regression.
==========================================================
17.) Close relationship between equine and human molluscum contagiosum virus demonstrated by in situ hybridisation.
==========================================================
Thompson CH1, Yager JA, Van Rensburg IB.
Author information
1
Department of Infectious Diseases, Faculty of Medicine, The University of Sydney, Australia.
Abstract
To determine whether the virus responsible for human molluscum contagiosum (MCV) is the causal agent of a similar disease in horses, in situ hybridisations using cloned fragments of human MCV DNA labelled with digoxigenin were carried out on formalin-fixed biopsy sections of lesions from two horses with molluscum contagiosum-like skin lesions. In both instances there was evidence of specific hybridisation of the labelled probe to target DNA in the sections under high stringency conditions, identified by the development of a deep blue-purple stain in the cytoplasm of cells in the stratum spinosum and stratum granulosum of the lesions and the absence of non-specific hybridisation in adjacent non-lesional areas of the epidermis. These results indicate that on the basis of very close homology of their viral DNA sequences, the causative virus of equine molluscum contagiosum is either identical with, or very closely related to, its human equivalent.
==========================================================
18.) Topical 20% KOH--an effective therapeutic modality for moluscum contagiosum in children.
==========================================================
Indian J Dermatol Venereol Leprol. 2003 Mar-Apr;69(2):175-7.
Mahajan BB1, Pall A, Gupta RR.
Author information
1
Dept. of Dermatology, Govt. Medical College & Hospital, Faridhot, Punjab.
Abstract
Topically 20% KOH aqueous solution once daily at bedtime was applied in 27 children having molluscum contagiosum by their parents, till lesions showed signs of inflammation or superficial ulceration. 24 children (88.9%) completed the trial and complete clearance was achieved after a mean period of 17 days. No recurrence was observed during follow up period. Thus in this open trial topical 20% KOH aqueous solution has proved to be convenient, easy to apply at home, safe and inexpensive alternative therapeutic modality for the treatment of molluscum contagiosum in children.
==========================================================
19.) Treatment of pediatric molluscum contagiosum with 10% potassium hydroxide solution.
==========================================================
J Dermatolog Treat. 2014 Jun;25(3):246-8. doi: 10.3109/09546634.2012.697988. Epub 2012 Jul 25.
Can B1, Topaloğlu F, Kavala M, Turkoglu Z, Zindancı I, Sudogan S.
Author information
1
Department of Dermatology, University of Medeniyet Goztepe Training and Research Hospital , Istanbul , Turkey.
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is a common cutaneous viral infection of the skin that is frequently seen in children. Although lesions can resolve spontaneously, treatment is mandatory because of the psychological effect of widespread lesions in children. Potassium hydroxide (KOH) is a strong alkali that has been used by dermatologists for a long time in identifying the fungal infections from skin scrapings.
AIMS:
We evaluated 40 children with MC for the safety and efficacy of treatment with topical 10% KOH aqueous solution.
METHODS:
Parents were instructed to apply a 10% KOH aqueous solution, twice daily, with a cotton stick to all lesions. Treatment was continued till the lesions showed signs of inflammation or superficial ulceration. Assessments of response and side effects were performed at the end of week 2, week 4, week 8 and week 12.
RESULTS:
We found complete clearance of lesions in 37 (92.5%) patients receiving topical 10%KOH solution after a mean period of four weeks. Three children dropped out of the study; two children reported severe stinging of the lesions and discontinued the treatment; the other patient developed hypopigmentation during the treatment. Local side effects were observed in 12 children (32.4%).
CONCLUSION:
Even though 10% KOH solution is associated with some local side effects, it is a safe, effective, inexpensive and noninvasive alternative treatment of MC in children.
==========================================================
20.) Topical salicylic acid gel as a treatment for molluscum contagiosum in children.
==========================================================
J Dermatolog Treat. 2005;16(5-6):336-40.
Leslie KS1, Dootson G, Sterling JC.
Author information
1
Department of Dermatology, Norfolk & Norwich University Hospital, Norwich, UK. kieronleslie@doctors.org.uk
Abstract
OBJECTIVE:
To determine if the application of salicylic acid gel or phenol solution affected resolution of molluscum contagiosum (MC) lesions in children.
PATIENTS AND METHODS:
This was a randomized, prospective controlled trial with two treatment arms and one vehicle arm for treatment of MC in children. The trial was set in the dermatology outpatient clinics of a teaching hospital and a district general hospital. A total of 114 children were enrolled in the study (age range 1-15 years) over a 4-year period; 83 of the children completed the study. Patients were randomized to receive one of three possible treatments: monthly vehicle application of 70% alcohol, monthly application of 10% phenol in 70% alcohol once or twice weekly 12% salicylic acid gel. All patients also received treatment with daily aqueous cream to reduce eczema. They returned monthly to the clinic for treatment and counting of MC lesions. They were reviewed either until complete resolution or up to 6 months, whichever occurred sooner. The main outcome measure was the time taken for complete resolution of MC lesions.
RESULTS:
In the intention-to-treat analysis there was no difference between treatment arms when the 31 non-completers were analysed as failures (log-rank test: p = 0.38). In an 'as treated' analysis, 16 of 27 children (59.2%: 95% confidence interval 30.2-88.3) had cleared with vehicle, 18 of 32 (56.3%, 30.3-82.2) with phenol solution and 21 of 24 (87.5%, 50.1-124.9) with salicylic acid gel (log-rank test: p = 0.03). On an as treated basis, salicylic acid was significantly better at clearing MC than dilute phenol (p = 0.006). The treatment in all groups was very well tolerated or acceptable in 93% of children.
CONCLUSION:
Our results suggest that topical salicylic acid may be beneficial in speeding resolution of MC in children. Dilute phenol application does not appear to affect the disease course.
==========================================================
21.) Essential oil of Australian lemon myrtle (Backhousia citriodora) in the treatment of molluscum contagiosum in children.
======== ==================================================
Biomed Pharmacother. 2004 May;58(4):245-7.
Burke BE1, Baillie JE, Olson RD.
Author information
1
Cardiovascular Section, Center for Biomedical Research, Inc., 2572 Waterbury lane, Boise, ID 83706-4980, USA. drq10@iglide.net
Abstract
Molluscum contagiosum is a common viral illness of childhood and is increasingly found as a sexually transmitted disease in sexually active young adults. Current treatment options are invasive, requiring tissue destruction and attendant discomfort. Thirty-one children (mean age 4.6 +/- 2.1 years) with the diagnosis of molluscum contagiosum (mean length of time with condition 8.6 +/- 5.3 months) were treated with once daily topical application of a 10% solution (v/v) of essential oil of Australian lemon myrtle (Backhousia citriodora) or vehicle (olive oil). At the end of 21 days, there was greater than 90% reduction in the number of lesions in 9/16 children treated with lemon myrtle oil, while 0/16 children met the same criteria for improvement in the vehicle group (P < 0.05). No adverse events were reported.
==========================================================
22.) Modified curettage technique for molluscum contagiosum.
==========================================================
Pediatr Dermatol. 2007 Mar-Apr;24(2):192-4.
Martín-García RF1, García ME, Rosado A.
Author information
1
Department of Dermatology, Medical Sciences Campus, University of Puerto Rico, Puerto Rico. martinmubarak@aol.com
Abstract
Molluscum contagiosum is a frequently occurring, virally induced cutaneous condition that affects infants, children, and adults. Although historically considered a self-limiting entity, many patients experience prolonged infections, often resistant to varied therapeutic interventions. Topical treatments achieve complete clearance in only a limited number of patients. Because of the associated pain, affected children are characteristically uncompliant to commonly used destructive modalities. We describe a modification of the traditional curettage technique to remove lesions of molluscum contagiosum, which has proven to be effective and well tolerated by a significant number of patients in our practice.
==========================================================
23.) Curettage treatment for molluscum contagiosum: a follow-up survey study.
==========================================================
Simonart T1, De Maertelaer V.
Author information
1
Department of Dermatology, Erasme University Hospital, 808 Route de Lennik, B-1070 Brussels, Belgium. tsimonar@ulb.ac.be
Abstract
BACKGROUND:
Although curettage is commonly used to treat molluscum contagiosum, prospective studies on its effectiveness are lacking.
OBJECTIVES:
To evaluate prospectively the efficacy of curettage in the treatment of molluscum contagiosum and to identify the risk factors associated with treatment failure.
METHODS:
A systematic 2-month follow-up survey study was carried out on 73 patients treated by curettage for molluscum contagiosum.
RESULTS:
Treatment of molluscum contagiosum by curettage was associated with a high risk of treatment failure at week 4 (42/64, 66%) and at week 8 (25/55, 45%). Risk factors for treatment failure at week 4 and 8 were the number of lesions at day 0 (P < 0.001), the number of involved anatomical sites (P < 0.001) and concomitant atopic dermatitis (P = 0.038 and P < 0.001, at weeks 4 and 8, respectively).
CONCLUSIONS:
The main risk factor for treatment failure is lesion number, underlining the importance of the early detection of the lesions or, alternatively, emphasizing the need for therapeutic options other than curettage in patients with numerous lesions.
==========================================================
24.) An open, comparative study of 10% potassium hydroxide solution versus salicylic and lactic acid combination in the treatment of molluscum contagiosum in children.
===========================================================
J Dermatolog Treat. 2013 Aug;24(4):300-4. doi: 10.3109/09546634.2011.649690. Epub 2012 Jan 31.
Köse O1, Özmen İ, Arca E.
Author information
1
Department of Dermatology, Gulhane School of Medicine, Ankara, Turkey. okose@gata.edu.tr
Abstract
OBJECTIVES:
To evaluate and compare the safety and efficacy of 10% potassium hydroxide (KOH) solution and salicylic and lactic acid (SAL + LAC) combination in the treatment of molluscum contagiosum (MC).
MATERIAL AND METHODS:
26 patients with MC randomized into two treatment groups. 12 patients treated with 10% KOH solution and 14 patients treated with SAL + LAC combination for 6 weeks. Parents of patients were instructed to apply medication once daily only to lesions at study onset. Assessment of response of the treated lesions and side effects was performed at 2, 4 and 6 weeks of the treatment. Newly acquired lesions were not included in the study.
RESULTS:
At the end of therapy, 83.3% (n = 10) of KOH group demonstrated complete remission and 16.7% (n = 2) of them showed partial remission; four patients (33%) developed new lesions during the study. All the patients in the SAL + LAC combination group (100%) demonstrated complete remission of study entry lesions at the end of 6 weeks with five patients (35%) acquiring new lesions during the study. Minor side effects were observed in two groups.
CONCLUSIONS:
10% KOH solution and SAL + LAC combination were found to be equally effective in the treatment of MC in children.
==========================================================
25.) Comparative study of 5 % potassium hydroxide solution versus 0.05% tretinoin cream for Molluscum Contagiosum in children.
==========================================================
Kathmandu Univ Med J (KUMJ). 2011 Oct-Dec;9(36):291-4.
Rajouria EA1, Amatya A, Karn D.
Author information
1
Department of Dermatology, Kathmandu University School of Medical Sciences, Dhulikhel Hospital- Kathmandu University Hospital, Dhulikhel, Nepal. eliz_aryal@yahoo.com
Abstract
BACKGROUND:
Molluscum contagiosum is one of the commonest cutaneous viral infections in children. All treatment modalities are associated with substantial pain, tissue destruction, and frequent recurrence.
OBJECTIVES:
To compare the efficacy and side effects of KOH 5% solution with tretinoin 0.05% cream for the treatment of molluscum contagiosum in children.
METHODS:
Fifty patients were randomly divided into 2 groups; 25 each for 5% KOH solution and 0.05% tretinoin cream. The given medication was applied at bed time over molluscum lesions. The assessment of response and side effects were performed weekly for 4 weeks.
RESULTS:
At the end of 4 weeks, the mean lesion count decreased from 9.48 +/- 3.00 SD to 1.67 +/- 0.58 SD and from 8.35 +/- 2.82 SD to 2.00 +/- 1.00 SD in patients treated with 5% KOH solution and 0.05% tretinoin cream respectively.
CONCLUSION:
The result of both KOH and tretinoin showed good response, well tolerated by children but between the two, KOH showed fast recovery and most lesions were resolved before 4 week. The side effects could be minimized if applied as stated above. On the other hand, tretinoin showed delayed response and even some of lesion extended beyond 4 week but the side effect were less, and hence can be used in recurrent cases.
==========================================================
26.) A comparative study of 10% KOH solution and 5% imiquimod cream for the treatment of Molluscum contagiosum in the pediatric age group.
==========================================================
Indian Dermatol Online J. 2015 Mar-Apr;6(2):75-80. doi: 10.4103/2229-5178.153005.
Chathra N1, Sukumar D1, Bhat RM1, Kishore BN1, Martis J1, Kamath G1, Srinath MK1, Monteiro R1.
Author information
1
Department of Dermatology, Venereology and Leprosy, Father Muller Medical College and Hospital, Kankanady, Mangalore, Karnataka, India.
Abstract
BACKGROUND:
Although Molluscum contagiosum (MC) is a self-limiting condition, active therapy could prevent further spread and improve cosmesis. Most of the available treatment modalities traumatize the lesions and have to be undertaken in the hospital, therefore evoking panic in children. In the quest for an alternative therapy, this study comparing 10% potassium hydroxide (KOH) solution and 5% imiquimod cream was taken up.
AIMS AND OBJECTIVES:
To compare the efficacy and tolerability of 10% KOH and 5% imiquimod in the treatment of MC.
MATERIALS AND METHODS:
This comparative study was conducted over a period of 18 months from October 2011 to March 2013, 40 patients between the age group of 1-18 years with clinically diagnosed MC were divided into two groups (lottery method), 20 patients were treated with 5% imiquimod cream (Group A) and the other 20 were treated with 10% KOH solution (Group B). Patients were followed up on the 4(th), 8(th) and 12(th) week of treatment.
RESULTS:
At the end of 12 weeks, out of 20 patients who received 10% KOH, 17 patients showed complete disappearance, whereas out of 20 patients who received 5% imiquimod, only 10 patients showed total clearance of the lesions. Adverse events were more frequent with 10% KOH, pigmentary disturbances being the most common.
CONCLUSION:
With only minor adverse effects, 10% KOH is an inexpensive and efficient modality for the treatment of MC in the pediatric age group. Although 5% imiquimod was effective in clearing the lesions with minimal adverse effects, the longer duration required for its efficacy may deter its wider use.
==========================================================
27.) Comparative study on the efficacy, safety, and acceptability of imiquimod 5% cream versus cryotherapy for molluscum contagiosum in children.
===========================================================
Pediatr Dermatol. 2010 Jul-Aug;27(4):388-94. doi: 10.1111/j.1525-1470.2009.00974.x. Epub 2010 Oct 4.
Al-Mutairi N1, Al-Doukhi A, Al-Farag S, Al-Haddad A.
Author information
1
Department of Dermatology & Venereology, Farwaniya Hospital, Farwaniya, Kuwait. nalmut@usa.net
Abstract
To compare the efficacy, safety and acceptability of imiquimod (IMQ) 5% cream with cryotherapy for the treatment of molluscum contagiosum (MC) in children. Prospective, randomized, comparative, observer blinded study. A total of 74 children, with MC were divided randomly to receive treatment with either IMQ 5% cream (group A) 5 days a week or cryotherapy (group B) once a week until clinical cure or up to a maximum of 16 weeks. All the patients were followed up weekly during active treatment. The patients were followed-up for 6 months after clinical cure to look for recurrence. In the IMQ group (group A), the overall complete cure rate was 91.8% (34 of 37), 22 of the 37 patients cleared by the end of 6 weeks and 12 more patients cleared by the end of 12 weeks, while the remaining three patients (8.1%) did not clear even after 16 weeks. Whereas, in the cryotherapy group, all 37 patients achieved complete cure, 26 of 37 (70.27%) patients cleared after 3 weeks, and the remaining 11 (29.72%) cleared by the end of 6 weeks. No statistically significant difference was found between the overall complete cure rate in both groups at the end of maximum treatment period (16 weeks). Pain, bullae formation, pigmentary changes, and superficial scarring were more significantly common in the cryotherapy group compared with the IMQ group. Imiqimod 5% cream seems to be slow acting but an effective agent for the treatment of MC in children. IMQ appears to be practically painless and more cosmetically accepted treatment when compared with cryotherapy, and may be the preferred treatment of MC in children especially with numerous small lesions. Cryotherapy has the advantage of being rapidly effective, and is less expensive than IMQ and may be the preferred treatment for large solitary or few lesions.
==========================================================
28.) Topical 0.3% and 0.5% podophyllotoxin cream for self-treatment of molluscum contagiosum in males. A placebo-controlled, double-blind study.
===========================================================
Dermatology. 1994;189(1):65-8.
Syed TA1, Lundin S, Ahmad M.
Author information
1
Department of Clinical Physiology, Malmö University Hospital, University of Lund, Sweden.
Abstract
BACKGROUND:
Molluscum contagiosum is generally a self-limiting benign skin disease that affects mostly children and young adults.
OBJECTIVE:
The purpose of this multicenter, double-blind, placebo-controlled study was to compare the clinical efficacy and tolerance of 0.3% and 0.5% podophyllotoxin in a hydrophilic cream base to cure molluscum contagiosum in Asian males.
METHODS:
Preselected patients (n = 150), age range 10-26 years (mean: 15.4), harboring 1,125 lesions (mean: 7.5), with size ranging from 2 to 8 mm in diameter (mean spot size 3.2 mm) and biopsy-proven diagnosis of molluscum contagiosum, were randomly allocated to three parallel groups. Twenty-four (16%) patients had atopic dermatitis. Patients self-administered placebo, 0.3% or 0.5% podophyllotoxin cream, twice daily for 3 consecutive days, and if total elimination was not achieved with one trial (6 topical applications), the same treatment was extended to 3 more weeks (24 topical applications in 4 weeks). The duration of the study was 12 weeks with 6 months (on monthly basis) follow-up. By the end of the treatment 80 patients (52, 92 and 16% patients in the 0.3%, 0.5% and the placebo groups, respectively) were evaluated as completely cured. During the treatment 92 patients (61.3%) did not complain of any allergic or localized adverse symptoms. Tolerable moderate to mild frequent side effects were pruritus (20.6%) and erythema (18%), with no dropouts. No recurrence was seen after 9 months of follow-up. Response to the trial medications appeared to be directly proportional to the concentration of podophyllotoxin (p < 0.001). Self-medication was well accepted by all the patients. It was concluded that the 0.5% podophyllotoxin cream preparation was more efficacious than the 0.3% incorporation (p < 0.001) and can be considered a safe, home-based first line of therapy to cure molluscum contagiosum.
==========================================================
29.) Comparative study of 5% and 2.5% potassium hydroxide solution for molluscum contagiosum in children.
===========================================================
Cutan Ocul Toxicol. 2014 Mar;33(1):54-9. doi: 10.3109/15569527.2013.796479. Epub 2013 May 29.
Uçmak D1, Akkurt MZ, Kacar SD, Sula B, Arica M.
Author information
1
Department of Dermatology, Dicle University , Diyarbakir , Turkey and.
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is a pediatric viral infection that is fairly contagious. Although various treatment methods are available, the presence of facial lesions limits options of therapy.
AIM:
We aimed to test an alternative treatment consisting of application of two different concentrations of potassium hydroxide (of KOH 5% solution and of KOH 2.5% solution) aqueous solution.
METHODS:
In this study we evaluated the effectiveness and side-effects of daily applications of potassium hydroxide (KOH) aqueous solution at 2.5% and 5% concentrations, twice daily in 29 children with MC. Out of a total of 29 patients with molluscum contagiosum included in the study, 13 patients in the 2.5% KOH group and 12 patients in the KOH 5% group completed the study. Families were instructed to apply potassium hydroxide twice a day. The assessment of response and side-effects were performed on days 0, 15, 30, 45 and 60 (visits were numbered 1, 2, 3, 4 and 5, respectively) and one month after.
RESULTS:
We had a total of 11 (44%) patients who completely recovered after the fifth visit. While eight (66.7%) of these 11 patients were in the 5% treatment group, three (23.1%) patients were in the 2.5% treatment group, and there was a statistically meaningful difference (p < 0.047). Patients with fewer lesions remitted better (p < 0.05). When number of lesions were taken into consideration, difference between the two treatment groups appeared after the fourth visit (p < 0.001). There were no statistical differences between the two groups with respect to side-effects (p = 0.682).
CONCLUSIONS:
Potassium hydroxide solution at a concentration of 5% was more effective than 2.5% in our patients. The treatment was well-tolerated on the face with the advantage of administration of lower concentrations. This study suggests potassium hydroxide may be a more preferable mode of treatment for molluscum contagiosum lesions on the face.
==========================================================
30.) Combination topical treatment of molluscum contagiosum with cantharidin and imiquimod 5% in children: a case series of 16 patients.
==========================================================
Australas J Dermatol. 2004 May;45(2):100-2.
Ross GL1, Orchard DC.
Author information
1
Dermatology Department, Royal Children's Hospital, Flemington Road, Parkville, Melbourne, Victoria 5052, Australia.
Abstract
The objective of this study was to assess the efficacy and tolerability of combination therapy for molluscum contagiosum (MC) with topical cantharidin and imiquimod 5%. A prospective case series of 16 paediatric patients with a mean age of 4.8 years had cantharidin applied to lesions by a dermatologist, followed by home treatment with imiquimod 5% cream nightly for an average of 5 weeks. This regimen resulted in >90% of lesions clearing in 12 patients, with half of these being totally clear. Two patients had 80-90% of lesions resolve. Two patients had 30-50% clearance of lesions at the end of the treatment period. One patient found the cantharidin reaction too strong. The mean number of imiquimod 250 mg sachets used was 4.25. In conclusion, this study suggests that combination therapy using cantharidin and imiquimod for treatment of MC in children is effective and well tolerated.
==========================================================
31.) Topical treatment of molluscum contagiosum with imiquimod 5% cream in Turkish children.
==========================================================
Pediatr Int. 2006 Aug;48(4):403-5.
Arican O1.
Author information
1
Department of Dermatology, Medical Faculty, Kahramanmaras Sutcuimam University, Kahramanmaras, Turkey. ozerari@gmail.com
Abstract
BACKGROUND:
Molluscum contagiosum (MC) is caused by a poxvirus which produces cutaneous lesions appearing as small, firm, umbilicated papules. Lesions of MC are most commonly seen in young children. Transmission is through viral particles, which remain on surfaces, autoinoculation, or from contact with open lesions. There are many options for treatment of MC and these may be broadly subdivided into destructive, immunological and antiviral therapies. An alternative treatment would be desirable in pediatric patients. Imiquimod (IQ) is a member of immune response modifiers.
METHODS:
Here, the results of 12 Turkish pediatric patients with MC who used IQ 5% cream (aged between 3-13 years; six boys, six girls) are given. The cream was applied by the mothers in the evening, three times per week every other day up to 16 weeks.
RESULTS:
One of the patients gave up the treatment because of Influenza-like symptoms, and two of them because of the progress in the lesions continued. In seven of the remaining nine patients, total recovery was achieved. Local side-effects in patients were well tolerated.
CONCLUSION:
When all the patients affected with MC who exclusively used IQ 5% cream as mentioned in the literature were studied, 35 of 83 patients (42.2%) had complete clearance. These have differences in the form and duration of application. IQ 5% cream can be preferred in the treatment of children with MC because of its applicability at home, easy application and good tolerability. However, different application methods and suitable treatment methods should be determined.
==========================================================
32.) Treatment of molluscum contagiosum with cantharidin: a practical approach.
==========================================================
Pediatr Ann. 2010 Mar;39(3):124-8, 130. doi: 10.3928/00904481-20100223-03.
Mathes EF1, Frieden IJ.
Author information
1
Department of Dermatology, University of California, San Francisco, USA. mathese@derm.ucsf.edu
Abstract
Molluscum contagiosum is very common. In this article we discuss the use of cantharidin as a treatment option for molluscum contagiosum and give detailed information about distribution sources, how to apply it, and caveats regarding its use.Molluscum contagiosum is a common viral disease of childhood caused by a poxvirus, which presents with small, firm, dome-shaped, umbilicated papules. It is generally benign and self-limited, with spontaneous resolution within 6 months to several years. Watchful waiting can often be an appropriate management strategy; however, some patients either desire or require treatment. Reasons for actively treating molluscum contagiosum may include alleviation of discomfort and itching (particularly in patients where an eczematous eruption - the so-called "molluscum eczema" - is seen in association) or in patients with ongoing atopic dermatitis where more lesions are likely to be present. Other reasons for treatment include limitation of spread to other areas and people, prevention of scarring and superinfection, and elimination of the social stigma of visible lesions. No one treatment is uniformly effective.Treatment options include destructive therapies (curettage, cryotherapy, cantharidin, and keratolytics, among others), immunomodulators (imiquimod, cimetidine, and Candida antigen), and antivirals (cidofovir). In this article we discuss and describe our first-line treatment approach for those molluscum needing treatment - cantharidin.
==========================================================
33.) Treatment of molluscum contagiosum with oral cimetidine: clinical experience in 13 patients.
==========================================================
Pediatr Dermatol. 1996 Jul-Aug;13(4):310-2.
Dohil M1, Prendiville JS.
Author information
1
British Columbia's Children's Hospital, Vancouver, Canada.
Abstract
Our purpose was to determine if oral cimetidine, a histamine-receptor antagonist, might be of benefit in the treatment of extensive molluscum contagiosum in children. We present 13 pediatric patients in whom conventional treatment modalities for molluscum contagiosum were unsuccessful or difficult to apply. They were treated with a two-month course of oral cimetidine 40 mg/kg/day. All but three children who completed treatment experienced clearance of all lesions. These children had no new lesions but had persistence of several lesions. One child did not take the drug and did not clear. No adverse effects were observed. We conclude that oral cimetidine may be of benefit in the management of widespread or facial molluscum contagiosum in immunocompetent children.
Comment in
==========================================================
34.) Treatment of molluscum contagiosum: a brief review and discussion of a case successfully treated with adapelene.
===========================================================
Dermatol Online J. 2007 Jul 13;13(3):15.
Scheinfeld N1.
Author information
1
Columbia University Department of Dermatology, USA.
Abstract
Molluscum contagiosum occur in 2-8 percent of children. This infection is among the most common viral skin infections in children. Although the lesions will resolve spontaneously when puberty, there are several reasons to treat them. The lesions can be cosmetically unappealing. About 10 percent of those with this infection develop a pruritic eczematous eruption. In about 4 percent of children with molluscum, the lesions are numerous and recurrent with no other coexisting immunological problem. Patients who have atopic dermatitis may develop widespread involvement with molluscum. Treatment options include destruction, topical therapy, and oral therapy. Destructive treatment modalities include curettage, cryotherapy, expression or pricking with a sterile needle, electrodesiccation, photodynamic therapy, and laser ablation. Destructive therapy is poorly tolerated in children. Topical medical therapy includes salicylic acid, glycolic acid, tretinoin, tazortene, 5 percent sodium nitrite co-applied daily with 5 percent salicylic acid topical preparations, podofilox, liquefied phenol, tretinoin, cantharidin, and potassium hydroxide. Oral treatment of molluscum includes cimetidine. No therapy is universally effective. I report herein a case of generalized numerous and recurrent molluscum treated with minimal irritation with adapelene.
==========================================================
35.) Interventions for cutaneous molluscum contagiosum.
==========================================================
van der Wouden JC1, van der Sande R, van Suijlekom-Smit LW, Berger M, Butler CC, Koning S.
Author information
1
Department of General Practice, Erasmus MC, University Medical Center, PO Box 1738, Rotterdam, Zuid-Holland, Netherlands, 3000 DR.
Abstract
BACKGROUND:
Molluscum contagiosum is a common skin infection, caused by a pox virus. The infection will usually resolve within months in people with a normal immune system. Many treatments have been used for molluscum contagiosum but a clear evidence base supporting them is lacking.This is an updated version of the original Cochrane Review published in Issue 2, 2006.
OBJECTIVES:
To assess the effects of management strategies (including waiting for natural resolution) for cutaneous, non-genital molluscum contagiosum in otherwise healthy people.
SEARCH STRATEGY:
In June 2009 we updated our searches of the Cochrane Skin Group Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (Issue 2, 2009), MEDLINE, EMBASE, and LILACS. We also searched ongoing trials registers, reference lists, and contacted pharmaceutical companies and experts in the field.
SELECTION CRITERIA:
We investigated randomised controlled trials (RCTs) for the treatment of molluscum contagiosum. We excluded trials on sexually transmitted molluscum contagiosum and in people with lowered immunity (including those with HIV infection).
DATA COLLECTION AND ANALYSIS:
Two authors independently selected studies, assessed methodological quality, and extracted data from selected studies.
MAIN RESULTS:
Eleven studies, with a total number of 495 participants, examined the effects of topical (9 studies), systemic, and homoeopathic interventions (1 study each). Limited evidence was found for the efficacy of sodium nitrite co-applied with salicylic acid compared to salicylic acid alone (risk ratio (RR) 3.50, 95% confidence interval (CI) 1.23 to 9.92); for Australian lemon myrtle oil compared to its vehicle, olive oil (RR 17.88, 95% CI 1.13 to 282.72); and for benzoyl peroxide cream compared to tretinoin (RR 2.20, 95% CI 1.01 to 4.79). No statistically significant differences were found for 10 other comparisons, most of which addressed 2 topical treatments.Study limitations included no blinding (four studies), many dropouts (three studies), and no intention-to-treat analysis; small study sizes may have led to important differences being missed. None of the evaluated treatment options were associated with serious adverse effects.
AUTHORS' CONCLUSIONS:
No single intervention has been shown to be convincingly effective in the treatment of molluscum contagiosum. The update identified six new studies, most of them reporting on interventions not included in the original version. However, the conclusions of the review did not change.
==========================================================
36.) Giant Molluscum Contagiosum in an HIV positive patient.
==========================================================
Int J Infect Dis. 2015 Sep;38:153-5. doi: 10.1016/j.ijid.2015.07.021. Epub 2015 Aug 6.
Pérez-Díaz CE1, Botero-García CA2, Rodríguez MC3, Faccini-Martínez ÁA4, Calixto OJ5, Benítez F5, Mantilla-Florez YF5, Bravo-Ojeda JS6, Espinal A6, Morales-Pertuz C6.
Author information
1
Servicios y Asesorías en Infectología (SAI), Bogotá, Colombia; Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia; Medicine school, Universidad Militar Nueva Granada, Bogotá, Colombia.
2
Medicine school, Universidad Militar Nueva Granada, Bogotá, Colombia.
3
Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia; Dermatology Department, Hospital Militar Central, Bogotá, Colombia.
4
Servicios y Asesorías en Infectología (SAI), Bogotá, Colombia; Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia. Electronic address: afaccini@gmail.com.
5
Servicios y Asesorías en Infectología (SAI), Bogotá, Colombia; Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia.
6
Tropical and Infectious Diseases Group (GETI), Hospital Militar Central, Universidad Militar Nueva Granada, Bogotá, Colombia; Internal Medicine department, Hospital Militar Central, Bogotá, Colombia.
Abstract
Molluscum Contagiosum (MC) is a skin infection caused by a double-stranded DNA virus of the family Poxviridae that replicates in the human epidermis, affecting mainly children and young sexually active adults and causing flesh colored papular lesions with central umbilication with an average size of 3-5mm, although atypical lesions that reach great size (Giant Molluscum Contagiosum), 10-15mm, can be seen in almost any immunodeficiency condition. We report the case of a 35 year old male patient with C3 HIV disease with an abdominal pathology associated to skin lesions predominantly in the forehead and scalp that reached sizes over 5mm, diagnosed as Giant Molluscum Contagiosum by skin biopsies.
==========================================================
37.) Giant molluscum contagiosum: an unusual presenting complaint of paediatric HIV disease.
==========================================================
Trop Doct. 2015 Apr;45(2):148-50. doi: 10.1177/0049475514568133. Epub 2015 Jan 18.
Chatterjee S1, Banerjee M2, Bhattacharya S3.
Author information
1
Resident, Department of Paediatrics, Medical College, Kolkata, India sayanchat_82@yahoo.co.in.
2
Resident, Department of Paediatrics, Medical College, Kolkata, India.
3
Associate Professor, Department of Paediatrics Medical College, Kolkata, India.
Abstract
We report a widely disseminated, disfiguring facial molluscum contagiosum (MC) as a presenting complaint in an 11-year-old girl secondary to human immune-deficiency virus infection. A biopsy specimen demonstrated lobulated epidermal growth consisting of keratinocytes with large intracytoplasmic eosinophilic inclusion bodies. The patient was treated with highly active anti-retroviral therapy (HAART). The extent of MC in our patient was remarkable and subsequently improved dramatically after starting HAART. Normally MC does not similarly respond in patients with AIDS.
==========================================================
38.) Generalized molluscum contagiosum in an HIV patient treated with diphencyprone.
==========================================================
J Dermatol Case Rep. 2010 Dec 31;4(4):60-2. doi: 10.3315/jdcr.2010.1059.
Chularojanamontri L1, Tuchinda P, Kulthanan K, Manuskiatti W.
Author information
1
Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand.
Abstract
BACKGROUND:
Diphencyprone is a universal contact immunotherapy. The mechanism of action is based on an induction of the delayed-type hypersensitivity. Diphencyprone has been used in various forms for treatments of recalcitrant and facial warts, and alopecia areata. However, this treatment modality has not been generally used in immunocompromised patients.
MAIN OBSERVATION:
The present report demonstrated the efficacy of diphencyprone immunotherapy on the treatment of generalized molluscum contagiosum in a human immunodeficiency virus (HIV)-infected patient. Minimal and transient side effects including pruritus, postinflammatory hyperpigmentation and irritation were noted.
CONCLUSION:
Diphencyprone contact immunotherapy appears to be a possible alternative treatment of widespread molluscum contagiosum in immunocompromised patients.
==========================================================
39.) Molluscum contagiosum effectively treated with a topical acidified nitrite, nitric oxide liberating cream.
==========================================================
Br J Dermatol. 1999 Dec;141(6):1051-3.
Ormerod AD1, White MI, Shah SA, Benjamin N.
Author information
1
Department of Dermatology, Aberdeen Royal Infirmary, Foresthill, UK. a.d.ormerod@abdn.ac.uk
Abstract
A double-blind, group-sequential clinical trial of acidified nitrite was performed to demonstrate the efficacy of this nitric oxide donor in treating molluscum contagiosum. Subjects received either 5% sodium nitrite co-applied with 5% salicylic acid under occlusion, or identical cream with 5% salicylic acid, omitting sodium nitrite. Active and control treatment groups were well matched for the number and duration of lesions and made a similar number of applications. We found a 75% cure rate in the active treatment group and 21% cure with control treatment (P = 0.01). The mean time to cure was 1.83 months. Staining of the skin and irritation were frequent side-effects but did not prevent successful treatment.
==========================================================
40.) Treatment of molluscum contagiosum with silver nitrate paste.
==========================================================
Pediatr Dermatol. 1999 Sep-Oct;16(5):395-7.
Niizeki K1, Hashimoto K.
Author information
1
Chigasaki Dermatology Clinic, Nanko, Japan.
Abstract
Three hundred eighty-nine consecutive patients with molluscum contagiosum were treated with 40% silver nitrate paste. The cure rate was 97.7% and no scars resulted.
==========================================================
41.) Efficacy of pulsed dyed laser (585 nm) in the treatment of molluscum contagiosum subtype 1.
==========================================================
Southeast Asian J Trop Med Public Health. 2007 Sep;38(5):849-54.
Chatproedprai S1, Suwannakarn K, Wananukul S, Theamboonlers A, Poovorawan Y.
Author information
1
Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
Abstract
Molluscum contagiosum is a common cutaneous disease that may be difficult to treat when there are multiple lesions; especially in children. This study was conducted to determine the efficacy of pulsed dye laser (585 nm) in the treatment of molluscum contagiosum in 20 children. In the treated group, 70.5% of lesions healed after the first treatment; the remaining 10.6% after the second treatment (2 weeks later). The overall cure rate was significantly different from the control group (p< 0.01). The therapy was also well tolerated. Only mild transient hypopigmentation and erythema were observed. None encountered infectious events. In conclusion, pulsed dye laser is a good alternative treatment for molluscum contagiosum due to high efficacy and mild transient side effects.
==========================================================
42.) Oral griseofulvin therapy in molluscum contagiosum.
==========================================================
Indian J Dermatol. 1987 Oct;32(4):104-6.
Mukul, Meena HS, Gupta S.
==========================================================
43.) [Molluscum contagiosum treated by topical using 10% tincture of iodine].
==========================================================
[Article in Chinese]
==========================================================
44.) Topical and intralesional cidofovir: a review of pharmacology
and therapeutic effects.
==========================================================
J Am Acad Dermatol. 1998 Nov;39(5 Pt 1):741-5.
Zabawski EJ Jr1, Cockerell CJ.
Author information
1
University of Texas Southwestern Medical Center, Dallas, USA.
Abstract
BACKGROUND:
Cidofovir is a potent nucleoside analog antiviral drug approved for the treatment of cytomegalovirus (CMV) retinitis in patients with AIDS. It is currently available only for intravenous infusion. Several small studies and case reports describe the successful use of cidofovir applied either topically or intralesionally in several virally induced cutaneous diseases.
OBJECTIVE:
Our purpose was to review the usefulness of topical and intralesional cidofovir for the treatment of viral infections caused by human papillomavirus, herpesviruses (including acyclovir-resistant strains), Kaposi's sarcoma-associated herpesvirus, and molluscum contagiosum.
METHODS:
We performed a review of recent literature.
RESULTS:
Cidofovir is a potent topical intralesional antiviral agent with activity against several DNA viruses that cause cutaneous disease. No significant systemic side effects have been noted, although application site reactions are common and can occasionally be severe.
CONCLUSION:
The effective use of topical and intralesional cidofovir for the treatment of diseases of the skin caused by DNA viruses has been demonstrated in a limited number of patients including those infected with HIV. Although larger studies will be necessary to determine the specific function that topical cidofovir will have in the treatment of cutaneous diseases caused by DNA viruses, the drug offers significant promise.
==========================================================
J Am Acad Dermatol. 1998 Nov;39(5 Pt 1):741-5.
Zabawski EJ Jr1, Cockerell CJ.
Author information
1
University of Texas Southwestern Medical Center, Dallas, USA.
Abstract
BACKGROUND:
Cidofovir is a potent nucleoside analog antiviral drug approved for the treatment of cytomegalovirus (CMV) retinitis in patients with AIDS. It is currently available only for intravenous infusion. Several small studies and case reports describe the successful use of cidofovir applied either topically or intralesionally in several virally induced cutaneous diseases.
OBJECTIVE:
Our purpose was to review the usefulness of topical and intralesional cidofovir for the treatment of viral infections caused by human papillomavirus, herpesviruses (including acyclovir-resistant strains), Kaposi's sarcoma-associated herpesvirus, and molluscum contagiosum.
METHODS:
We performed a review of recent literature.
RESULTS:
Cidofovir is a potent topical intralesional antiviral agent with activity against several DNA viruses that cause cutaneous disease. No significant systemic side effects have been noted, although application site reactions are common and can occasionally be severe.
CONCLUSION:
The effective use of topical and intralesional cidofovir for the treatment of diseases of the skin caused by DNA viruses has been demonstrated in a limited number of patients including those infected with HIV. Although larger studies will be necessary to determine the specific function that topical cidofovir will have in the treatment of cutaneous diseases caused by DNA viruses, the drug offers significant promise.
Producido Por Dr. Jose Lapenta R. Dermatologo
Maracay Estado Aragua Venezuela 2.017-2.023
Telf: 04142976087- 04127766810
04166401045
Follow @dermagicexpress



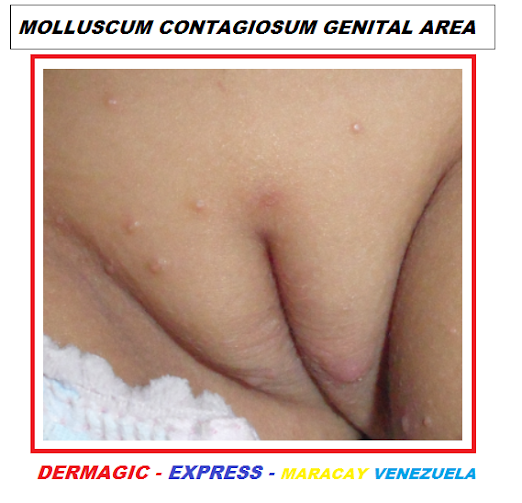



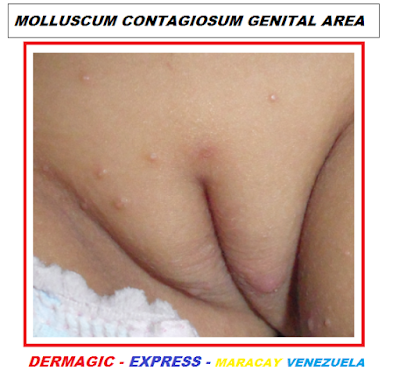


No hay comentarios:
Publicar un comentario
Tu comentario será objeto de revisión y luego aprobado.
Your comment will be revised and then approved.