La Pitiriasis Versicolor, Mitos, Historia y Tratamientos. !
The Pityriasis Versicolor, Myths, History, and Treatments. !
PITIRIASIS VERSICOLOR
PUBLICADO 2.016 ACTUALIZADO 2.023
EDITORIAL ESPAÑOL
=================
Hola amigos de la red, DERMAGIC EXPRESS hoy les trae un tema bien interesante, porque es muy común en la práctica médica dermatológica: LA PITIRIASIS VERSICOLOR, REVISION también conocida como TIÑA VERSICOLOR, enfermedad que en la antigüedad fue conocida bajo el nombre de "MANCHAS DEL HIGADO", por la creencia de que el daño hepático era el causal de ella.
Esta es la razón principal de esta Revisión Bibliográfica: la mayoría de los pacientes que acuden al médico piensan que esta enfermedad es producida por un "DAÑO HEPATICO" o abuso de alcohol, y el nombre de "MANCHAS DEL HIGADO" se lo colocaron porque el consumo de bebidas alcohólicas, por el efecto de vasodilatación en la piel, hace que las manchas se "noten" mas, eso es todo.
También son conocidas como "HONGO SOLAR" porque cuando la persona contaminada expone su piel al sol (PISCINA O PLAYA) se notan mas las lesiones, y realmente las manchas ya están allí, pero producen un efecto "PARAGUA" y la piel no se broncea en el área del hongo.
=================
Hola amigos de la red, DERMAGIC EXPRESS hoy les trae un tema bien interesante, porque es muy común en la práctica médica dermatológica: LA PITIRIASIS VERSICOLOR, REVISION también conocida como TIÑA VERSICOLOR, enfermedad que en la antigüedad fue conocida bajo el nombre de "MANCHAS DEL HIGADO", por la creencia de que el daño hepático era el causal de ella.
Esta es la razón principal de esta Revisión Bibliográfica: la mayoría de los pacientes que acuden al médico piensan que esta enfermedad es producida por un "DAÑO HEPATICO" o abuso de alcohol, y el nombre de "MANCHAS DEL HIGADO" se lo colocaron porque el consumo de bebidas alcohólicas, por el efecto de vasodilatación en la piel, hace que las manchas se "noten" mas, eso es todo.
También son conocidas como "HONGO SOLAR" porque cuando la persona contaminada expone su piel al sol (PISCINA O PLAYA) se notan mas las lesiones, y realmente las manchas ya están allí, pero producen un efecto "PARAGUA" y la piel no se broncea en el área del hongo.
PITIRIASIS VERSICOLOR SENOS MUJER
En 1.889 el científico ROBIN (Baillon) describió el agente causal
de esta patología LA MALASSEZIA FURFUR, también conocida hoy con el nombre de PITYROSPORUM ORBICULARE, y su otra variante PITYROSPORUM OVALE, un hongo superficial con gran afinidad por las "grasas de
la piel", lo cual significa que es LIPOFILICO. Este hongo una vez
contagiada la persona se instala o vive en el cuero cabelludo.
Recordemos que en años recientes se ha relacionado este hongo
con LA DERMATITIS SEBORREICA o "CASPA".
La enfermedad se manifiesta como unas "manchas" ovales de pequeño a mediano tamaño, las cuales pueden ser de varios colores: BLANCAS, ROSADAS Y MARRONES, de allí el nombre de VERSICOLOR, que significa "DE VARIOS COLORES", por lo general se presentan desde el área del cuero cabelludo, bajando por el cuello hombro, tórax y brazos. En algunos casos producen picazón o prurito, pero mayormente son asintomáticas.
La enfermedad se manifiesta como unas "manchas" ovales de pequeño a mediano tamaño, las cuales pueden ser de varios colores: BLANCAS, ROSADAS Y MARRONES, de allí el nombre de VERSICOLOR, que significa "DE VARIOS COLORES", por lo general se presentan desde el área del cuero cabelludo, bajando por el cuello hombro, tórax y brazos. En algunos casos producen picazón o prurito, pero mayormente son asintomáticas.
FORMA DE CONTAGIO: CONTACTO
DIRECTO de persona a persona, PISCINAS, PLAYAS, y elementos
contaminados con el hongo como ropa y toallas de baño.
DIAGNOSTICO DE LA PITIRIASIS VERSICOLOR:
=========================================
1.) CLINICAMENTE: el aspecto de las lesiones.
2.) SIGNO DE BESNIER: al rasparlas con la uña producen descamación.
3.) CINTA ADHESIVA: Consiste en colocar un teipe transparente "SCOTCH" sobre la lesión, retirarlo, pegarlo a una laminilla y observar al microscopio óptico las formas del hongo descritas como "espaguetis con bolas de carne o albóndigas"
4.) KOH: HIDROXIDO DE POTASIO AL 10%: o tinta AZUL PARKER, la cual se coloca en los bordes del teipe adherido a la lámina, esto permite mejor la visualización del hongo.
5.) LUZ DE WOOD: viejo método que data de 1.925 cuando los científicos MARGAROT Y DEVEZE descubrieron que la luz ultravioleta con un filtro de WOOD permitía ver "FLUORESCENCIA" en algunas enfermedades, en este caso: al colocar el paciente en un cuarto oscuro y alumbrarlo con la lámpara de Wood: las lesiones toman un color "VIOLETA". Esta lámpara es usada comúnmente hoy día para verificar "BILLETES FALSOS".
6.) CULTIVO: en la práctica diaria no se utiliza, su utilidad es desde el punto de vista científico para la tipificación del hongo y sus variantes, hoy día se describen más de 13 variantes de MALASSEZIA, siendo la FURFUR Y GLOBOSA, las más involucradas en el humano.
DIAGNOSTICO DIFERENCIAL:
=========================
LA PITIRIASIS VERSICOLOR SE PUEDE CONFUNDIR CON:
1.) LEPRA INDETERMINADA.
2.) PITIRIASIS ALBA.
3.) VITILIGO.
4.) PITIRIASIS ROSADA.
5.) DERMATITIS SEBORREICA.
6.) HIPOMELANOSIS MACULAR PROGRESIVA.
7.) ERITRASMA.
8.) SIFILIS.
No todas las personas expuestas al hongo se contaminan, y esto sucede porque la COMPOSICION QUIMICA DE LA PIEL, VARIA DE PERSONA A PERSONA, quiere decir esto que hay personas que NUNCA SUFRIRAN DE PITIRIASIS VERSICOLOR, aun teniendo familiares y personas cercanas con la enfermedad, pues su COMPOSICION LIPIDICA, de la piel no es afín con el hongo.
DIAGNOSTICO DE LA PITIRIASIS VERSICOLOR:
=========================================
1.) CLINICAMENTE: el aspecto de las lesiones.
2.) SIGNO DE BESNIER: al rasparlas con la uña producen descamación.
3.) CINTA ADHESIVA: Consiste en colocar un teipe transparente "SCOTCH" sobre la lesión, retirarlo, pegarlo a una laminilla y observar al microscopio óptico las formas del hongo descritas como "espaguetis con bolas de carne o albóndigas"
4.) KOH: HIDROXIDO DE POTASIO AL 10%: o tinta AZUL PARKER, la cual se coloca en los bordes del teipe adherido a la lámina, esto permite mejor la visualización del hongo.
5.) LUZ DE WOOD: viejo método que data de 1.925 cuando los científicos MARGAROT Y DEVEZE descubrieron que la luz ultravioleta con un filtro de WOOD permitía ver "FLUORESCENCIA" en algunas enfermedades, en este caso: al colocar el paciente en un cuarto oscuro y alumbrarlo con la lámpara de Wood: las lesiones toman un color "VIOLETA". Esta lámpara es usada comúnmente hoy día para verificar "BILLETES FALSOS".
6.) CULTIVO: en la práctica diaria no se utiliza, su utilidad es desde el punto de vista científico para la tipificación del hongo y sus variantes, hoy día se describen más de 13 variantes de MALASSEZIA, siendo la FURFUR Y GLOBOSA, las más involucradas en el humano.
DIAGNOSTICO DIFERENCIAL:
=========================
LA PITIRIASIS VERSICOLOR SE PUEDE CONFUNDIR CON:
1.) LEPRA INDETERMINADA.
2.) PITIRIASIS ALBA.
3.) VITILIGO.
4.) PITIRIASIS ROSADA.
5.) DERMATITIS SEBORREICA.
6.) HIPOMELANOSIS MACULAR PROGRESIVA.
7.) ERITRASMA.
8.) SIFILIS.
No todas las personas expuestas al hongo se contaminan, y esto sucede porque la COMPOSICION QUIMICA DE LA PIEL, VARIA DE PERSONA A PERSONA, quiere decir esto que hay personas que NUNCA SUFRIRAN DE PITIRIASIS VERSICOLOR, aun teniendo familiares y personas cercanas con la enfermedad, pues su COMPOSICION LIPIDICA, de la piel no es afín con el hongo.
PITIRIASIS VERSICOLOR GIGANTE EN ESPALDA DE MUJER
LOS TRATAMIENTOS MAS UTILIZADOS:
==================================
1.) HIPOSULFITO DE SODIO.
2.) TOLNAFTATO.
3.) KETOCONAZOL TABLETAS Y CHAMPU.
4.) TERBINAFINA.
5.) FLUCONAZOL.
6.) ITRACONAZOL.
7.) SERTACONAZOL.
8.) ACIDO SALICILICO
9.) FENOL.
10.) BIFONAZOL.
11.) SULFURO DE SELENIO CHAMPU y otros
De estos los más populares son KETOCONAZOL en tabletas y champú, ITRACONAZOLE, TERBINAFINA Y FOLUCONAZOL oral, Y SULFURO DE SELENIO champú.
Debes entender que una vez realizado el tratamiento debes exponer tu piel al sol: PISCINA O PLAYA, paradójicamente, PUES si la piel ya sana no recibe luz solar, tardara mas en tomar su coloración original. El hongo inhibe la coloración normal de la piel produciendo HIPOCROMIA RESIDUAL.
Esta enfermedad, siendo totalmente benigna suele RECAER CON FRECUENCIA y esto se debe al hecho que siempre tu piel estará expuesta al hongo en PISCINAS, PLAYAS, PERSONAS o ROPA contaminada, y ella por su composición química como te explique, en las personas afectadas tiene afinidad por el hongo.
Como mantenimiento luego de curar de la enfermedad te recomiendo utilizar un buen champú anti caspa que contenga un antimicótico como KETOCONAZOL, BIFONAZOL o SULFURO DE SELENIO, una o 2 veces semanal. Esto por el hecho que ya te explique, el hongo tiene su "HABITAT" en el cuero cabelludo.
En las referencias los hechos, en las fotos distintas formas DE LA PITIRIASIS VERSICOLOR.
Saludos a Todos.
Dr. José Lapenta.
Dr. José M. Lapenta
EDITORIAL ENGLISH
===================
Hello friends of the network, DERMAGIC EXPRESS today brings you a very interesting topic, because it is very common in the dermatological medical practice: PIYIRIASIS VERSICOLOR, A REVIEW, also known as TINEA VERSICOLOR, a disease that in ancient times was known as "LIVER SPOTS "because of the belief that liver damage was the cause of it.
This is the main reason for this Bibliographic Review: Most patients who come to the doctor think that this disease is caused by a "HEPATIC DAMAGE" or alcohol abuse, and the name "LIVER SPOTS" was placed because the Consumption of alcoholic beverages, by the effect of vasodilatation on the skin, makes the spots "notice" more, that's all.
They are also known as "SUN FUNGUS" because when the contaminated person exposes their skin to the sun (SWIMMING POOL or BEACH) the lesions are noticed, and indeed the spots are already there, but they produce a "UMBRELLA" effect and the skin does not tan In the mushroom area.
In 1.889 the scientist ROBIN (Baillon) described the causal agent of this pathology THE MALASSEZIA FURFUR, also known today as PITYROSPORUM ORBICULARE, and its other variant PITYROSPORUM OVALE, a superficial fungus with a great affinity for "skin fats”, which means that it is LIPOPHILIC. This fungus once infected the person is settled or lives on the scalp. Recall that in recent years this fungus has been linked with SEBORRHEIC DERMATITIS or "DANDRUFF".

The disease manifests itself as an oval "spot" of small to medium size, which can be of several colors: WHITE, PINK AND BROWN, hence the name VERSICOLOR, which means "OF VARIOUS COLORS", usually presented From the scalp area, down the neck shoulder, thorax and arms. In some cases itchy or pruritus, but mostly they are asymptomatic.
CONTAGIUM FORMS: DIRECT CONTACT from person to person, POOLS, BEACHES, and elements contaminated with the fungus as clothes and bath towels.
DIAGNOSIS OF PITYRIASIS VERSICOLOR:
====================================
1.) CLINICALLY: the appearance of the lesions.
2.) BESNIER SIGN: Scraping them with the nail causes desquamation.
3.) ADHESIVE TAPE: Consists of placing a transparent "SCOTCH" tape on the lesion, removing it, gluing it to a glass sheet and observing under the light microscope the forms of the fungus described as "spaghetti with meatballs"
4.) KOH: 10% POTASSIUM HYDROXIDE: or PARKER BLUE ink, which is placed on the edges of the tape attached to the sheet, this allows better visualization of the fungus.
5.) WOOD LIGHT: Old method dating back to 1.925 when scientists MARGAROT and DEVEZE discovered that ultraviolet light with a WOOD filter made it possible to see "FLUORESCENCE" in some diseases, in this case: when placing the patient in a dark room and light it with the lamp of Wood: the lesions take a "VIOLET" color. This lamp is commonly used today to check "FALSE TICKETS".
5.) CULTIVATION: in the daily practice is not used, its usefulness is from the scientific point of view for the typification of the fungus and its variants, today more than 13 variants of MALASSEZIA are described, being FURFUR AND GLOBOSA, the most Involved in the human.
===================
Hello friends of the network, DERMAGIC EXPRESS today brings you a very interesting topic, because it is very common in the dermatological medical practice: PIYIRIASIS VERSICOLOR, A REVIEW, also known as TINEA VERSICOLOR, a disease that in ancient times was known as "LIVER SPOTS "because of the belief that liver damage was the cause of it.
This is the main reason for this Bibliographic Review: Most patients who come to the doctor think that this disease is caused by a "HEPATIC DAMAGE" or alcohol abuse, and the name "LIVER SPOTS" was placed because the Consumption of alcoholic beverages, by the effect of vasodilatation on the skin, makes the spots "notice" more, that's all.
They are also known as "SUN FUNGUS" because when the contaminated person exposes their skin to the sun (SWIMMING POOL or BEACH) the lesions are noticed, and indeed the spots are already there, but they produce a "UMBRELLA" effect and the skin does not tan In the mushroom area.
In 1.889 the scientist ROBIN (Baillon) described the causal agent of this pathology THE MALASSEZIA FURFUR, also known today as PITYROSPORUM ORBICULARE, and its other variant PITYROSPORUM OVALE, a superficial fungus with a great affinity for "skin fats”, which means that it is LIPOPHILIC. This fungus once infected the person is settled or lives on the scalp. Recall that in recent years this fungus has been linked with SEBORRHEIC DERMATITIS or "DANDRUFF".

The disease manifests itself as an oval "spot" of small to medium size, which can be of several colors: WHITE, PINK AND BROWN, hence the name VERSICOLOR, which means "OF VARIOUS COLORS", usually presented From the scalp area, down the neck shoulder, thorax and arms. In some cases itchy or pruritus, but mostly they are asymptomatic.
CONTAGIUM FORMS: DIRECT CONTACT from person to person, POOLS, BEACHES, and elements contaminated with the fungus as clothes and bath towels.
DIAGNOSIS OF PITYRIASIS VERSICOLOR:
====================================
1.) CLINICALLY: the appearance of the lesions.
2.) BESNIER SIGN: Scraping them with the nail causes desquamation.
3.) ADHESIVE TAPE: Consists of placing a transparent "SCOTCH" tape on the lesion, removing it, gluing it to a glass sheet and observing under the light microscope the forms of the fungus described as "spaghetti with meatballs"
4.) KOH: 10% POTASSIUM HYDROXIDE: or PARKER BLUE ink, which is placed on the edges of the tape attached to the sheet, this allows better visualization of the fungus.
5.) WOOD LIGHT: Old method dating back to 1.925 when scientists MARGAROT and DEVEZE discovered that ultraviolet light with a WOOD filter made it possible to see "FLUORESCENCE" in some diseases, in this case: when placing the patient in a dark room and light it with the lamp of Wood: the lesions take a "VIOLET" color. This lamp is commonly used today to check "FALSE TICKETS".
5.) CULTIVATION: in the daily practice is not used, its usefulness is from the scientific point of view for the typification of the fungus and its variants, today more than 13 variants of MALASSEZIA are described, being FURFUR AND GLOBOSA, the most Involved in the human.
DIFFERENTIAL DIAGNOSIS:
========================
THE PITYRIASIS VERSICOLOR CAN BE CONFUSED WITH:
1.) LEPROSY.
2.) PITYIRIASIS ALBA.
3.) VITILIGO.
4.) PIYIRIASIS ROSEA
5.) SEBORRHEIC DERMATITIS.
6.) PROGRESSIVE MACULAR HYPOMELANOSIS.
7.) ERYTHRASMA.
8.) SYPHILIS.
Not all people exposed to the fungus are contaminated, and this happens because the CHEMICAL COMPOSITION OF THE SKIN, IS DIFFERENT FROM PERSON TO PERSON, means that there are people who WILL NEVER SUFFER FROM PITYRIASIS VERSICOLOR, even having relatives and people close with the disease, because it’s LIPHIDIC COMPOSITION, of the skin is not related to the fungus.
THE MOST USED TREATMENTS:
===========================
1.) SODIUM HYPOSULPHITE.
2.) TOLNAFTATE.
3.) KETOCONAZOLE TABLETS AND SHAMPOO.
4.) TERBINAFINE.
5.) FLUCONAZOLE.
6.) ITRACONAZOLE.
7.) SERTACONAZOLE.
8.) SALICYLIC ACID
9.) PHENOL.
10.) BIFONAZOLE
11.) SELENIUM SULFIDE SHAMPOO and others.
You must understand that once the treatment is done you should expose your skin to the sun: POOL OR BEACH, paradoxically, BECAUSE if the already healthy skin does not receive sunlight, it will take longer to take its original coloration. The fungus inhibits the normal coloration of the skin producing RESIDUAL HYPOCROMY.
This disease, being totally benign, is often RELAPSE WITH FREQUENCY and this is due to the fact that your skin will always be exposed to the fungus in SWIMMING POOLS, BEACHES, PEOPLE or contaminated CLOTHING, and it why its chemical composition as explain it, in the affected people it has affinity By the fungus.
As maintenance after curing the disease I recommend using a good anti-dandruff shampoo containing an antimycotic like KETOCONAZOLE, BIFONAZOLE or SELENIUM SULFIDE, once or twice weekly. This because of the fact that already explained to you, the fungus has its "HABITAT" on the scalp.
In the references the facts, in the photos different forms OF PITYRIASIS VERSICOLOR.
Greetings to all.
Dr. José Lapenta.
THE PITYRIASIS VERSICOLOR CAN BE CONFUSED WITH:
1.) LEPROSY.
2.) PITYIRIASIS ALBA.
3.) VITILIGO.
4.) PIYIRIASIS ROSEA
5.) SEBORRHEIC DERMATITIS.
6.) PROGRESSIVE MACULAR HYPOMELANOSIS.
7.) ERYTHRASMA.
8.) SYPHILIS.
Not all people exposed to the fungus are contaminated, and this happens because the CHEMICAL COMPOSITION OF THE SKIN, IS DIFFERENT FROM PERSON TO PERSON, means that there are people who WILL NEVER SUFFER FROM PITYRIASIS VERSICOLOR, even having relatives and people close with the disease, because it’s LIPHIDIC COMPOSITION, of the skin is not related to the fungus.
THE MOST USED TREATMENTS:
===========================
1.) SODIUM HYPOSULPHITE.
2.) TOLNAFTATE.
3.) KETOCONAZOLE TABLETS AND SHAMPOO.
4.) TERBINAFINE.
5.) FLUCONAZOLE.
6.) ITRACONAZOLE.
7.) SERTACONAZOLE.
8.) SALICYLIC ACID
9.) PHENOL.
10.) BIFONAZOLE
11.) SELENIUM SULFIDE SHAMPOO and others.
Of these the most popular are KETOCONAZOLE in tablets and shampoo, oral
ITRACONAZOLE, TERBINAFINE, FLUCONAZOLE, and SELENIUM SULFIDE shampoo.
You must understand that once the treatment is done you should expose your skin to the sun: POOL OR BEACH, paradoxically, BECAUSE if the already healthy skin does not receive sunlight, it will take longer to take its original coloration. The fungus inhibits the normal coloration of the skin producing RESIDUAL HYPOCROMY.
This disease, being totally benign, is often RELAPSE WITH FREQUENCY and this is due to the fact that your skin will always be exposed to the fungus in SWIMMING POOLS, BEACHES, PEOPLE or contaminated CLOTHING, and it why its chemical composition as explain it, in the affected people it has affinity By the fungus.
As maintenance after curing the disease I recommend using a good anti-dandruff shampoo containing an antimycotic like KETOCONAZOLE, BIFONAZOLE or SELENIUM SULFIDE, once or twice weekly. This because of the fact that already explained to you, the fungus has its "HABITAT" on the scalp.
In the references the facts, in the photos different forms OF PITYRIASIS VERSICOLOR.
Greetings to all.
Dr. José Lapenta.
Dr. José M. Lapenta.
=========================================================================
REFERENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
=========================================================================
REFERENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
=========================================================================
1.) [Pityriasis versicolor in infants: unusual clinical presentation and
role of corticosteroids used as depigmenting agent for cosmetic purposes in
the mother].
2.) Folliculocentric tinea versicolor.
3.) Comparative efficacy of topical application of tacrolimus and clotrimazole in the treatment of pityriasis versicolor: A single blind, randomised clinical trial.
4.) Comparative clinical trial: fluconazole alone or associated with topical ketoconazole in the treatment of pityriasis versicolor.
6.) Comparison between fluconazole and ketoconazole effectivity in the treatment of pityriasis versicolor.
7.) Treatment of pityriasis versicolor with topical application of essential oil of Cymbopogon citratus (DC) Stapf - therapeutic pilot study.
8.) Atrophying pityriasis versicolor as an idiosyncratic T cell-mediated response to Malassezia: A case series.
9.) Progress in Malassezia Research in Korea.
10.) Malassezia species in healthy skin and in dermatological conditions.
11.) Targeting Malassezia species for novel synthetic and natural antidandruff agents.
12.) Biofilm, adherence, and hydrophobicity as virulence factors in Malassezia furfur.
13.) Antifungal susceptibility testing of Malassezia spp. with an optimized colorimetric broth microdilution method.
14.) Pityriasis versicolor: an update on pharmacological treatment options.
15.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
16.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
17.) Mycological Considerations in the Topical Treatment of Superficial Fungal Infections.
18.) Single-dose fluconazole versus itraconazole in pityriasis versicolor.
19.) Itraconazole in tinea versicolor: a review.
20.) [Cutaneous Malassezia infections and Malassezia associated dermatoses: An update].
21.) A double-blind comparative study of sodium sulfacetamide lotion 10% versus selenium sulfide lotion 2.5% in the treatment of pityriasis (tinea) versicolor.
22.) Selenium sulfide in tinea versicolor: blood and urine levels.
23.) New Antifungal Agents and New Formulations Against Dermatophytes.
24.) Tavaborole, Efinaconazole, and Luliconazole: Three New Antimycotic Agents for the Treatment of Dermatophytic Fungi.
25.) Therapeutic efficacy and safety of the new antimycotic sertaconazole in the treatment of Pityriasis versicolor.
25.) Whole genome sequencing analysis of the cutaneous pathogenic yeast Malassezia restricta and identification of the major lipase expressed on the scalp of patients with dandruff.
26.) Rook, Arthur et all. Textbook of Dermatology. Blakwell Scientific Publicat. Oxford and Edinburgh 1968.
====================================================================
====================================================================
2.) Folliculocentric tinea versicolor.
3.) Comparative efficacy of topical application of tacrolimus and clotrimazole in the treatment of pityriasis versicolor: A single blind, randomised clinical trial.
4.) Comparative clinical trial: fluconazole alone or associated with topical ketoconazole in the treatment of pityriasis versicolor.
6.) Comparison between fluconazole and ketoconazole effectivity in the treatment of pityriasis versicolor.
7.) Treatment of pityriasis versicolor with topical application of essential oil of Cymbopogon citratus (DC) Stapf - therapeutic pilot study.
8.) Atrophying pityriasis versicolor as an idiosyncratic T cell-mediated response to Malassezia: A case series.
9.) Progress in Malassezia Research in Korea.
10.) Malassezia species in healthy skin and in dermatological conditions.
11.) Targeting Malassezia species for novel synthetic and natural antidandruff agents.
12.) Biofilm, adherence, and hydrophobicity as virulence factors in Malassezia furfur.
13.) Antifungal susceptibility testing of Malassezia spp. with an optimized colorimetric broth microdilution method.
14.) Pityriasis versicolor: an update on pharmacological treatment options.
15.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
16.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
17.) Mycological Considerations in the Topical Treatment of Superficial Fungal Infections.
18.) Single-dose fluconazole versus itraconazole in pityriasis versicolor.
19.) Itraconazole in tinea versicolor: a review.
20.) [Cutaneous Malassezia infections and Malassezia associated dermatoses: An update].
21.) A double-blind comparative study of sodium sulfacetamide lotion 10% versus selenium sulfide lotion 2.5% in the treatment of pityriasis (tinea) versicolor.
22.) Selenium sulfide in tinea versicolor: blood and urine levels.
23.) New Antifungal Agents and New Formulations Against Dermatophytes.
24.) Tavaborole, Efinaconazole, and Luliconazole: Three New Antimycotic Agents for the Treatment of Dermatophytic Fungi.
25.) Therapeutic efficacy and safety of the new antimycotic sertaconazole in the treatment of Pityriasis versicolor.
25.) Whole genome sequencing analysis of the cutaneous pathogenic yeast Malassezia restricta and identification of the major lipase expressed on the scalp of patients with dandruff.
26.) Rook, Arthur et all. Textbook of Dermatology. Blakwell Scientific Publicat. Oxford and Edinburgh 1968.
====================================================================
====================================================================
1.) [Pityriasis versicolor in infants: unusual clinical presentation and
role of corticosteroids used as depigmenting agent for cosmetic purposes in
the mother].
===========================================================
Pan Afr Med J. 2017 Jan 23;26:31. doi: 10.11604/pamj.2017.26.31.11504. eCollection 2017.
[Article in French]
Dioussé P1, Ly F2, Bammo M3, Lizia S2, Diallo TAA1, Dione H1, Sarr F1, Gueye RD1, Gueye AM1, Dieng MT2, Diop BM1, Ka MM1.
Author information
1
UFR des Sciences de la Santé, Université de Thiès, Sénégal.
2
Dermatologie, Université Cheikh Anta Diop, Dakar, Sénégal.
3
Dermatologie, Hôpital Régional de Thiès, Sénégal.
Abstract
We report two cases of Pityriasis versicolor (PV) in infants aged 12 and 18 months. The latter were brought to medical attention because of hypochromic and achromic, round macules involving the limbs and the face. Physical examination of their mothers showed voluntary depigmentation for cosmetic purposes due to the use of corticosteroids and hydroquinone, on average, over a 5-year period. The scotch tape test performed in one of the infants and his mother showed short filaments and clusters of spores. Treatment was based on ketoconazole. After 8 weeks, all patients reported favorable outcomes despite the persistence of some hypochomic macules. The peculiarities of this study are, on the one hand the topography of the lower limbs and on the other hand a positive family history of PV whose occurrence is favored by the use of depigmenting agents based on corticosteroids. Corticosteroids favor the atrophic and achromic feature of the lesions. Indeed, achromic lesions on the lower limbs were described in adults undergoing artificial depigmentation.
==========================================================
2.) Folliculocentric tinea versicolor.
==========================================================
Dermatol Online J. 2017 Feb 15;23(2). pii: 13030/qt5kj574bd.
Hudson A1, Carroll B, Kim SJ.
Author information
1
Department of Dermatology, Texas Tech University Health Sciences Center, Lubbock. andrew.hudson@ttuhsc.edu.
Abstract
Tinea versicolor (TV) is typically an asymptomatic fungal infection of the stratum corneum owing to Malassezia overgrowth. It presents as hypo or hyperpigmented macules with fine scale that coalesce into patches on the trunk, neck, and/or arms. Presented in this report is a 34-year-old man with an interesting case of folliculocentric tinea versicolor manifesting as perifollicular hypopigmented macules on the lower back.
==========================================================
3.) Comparative efficacy of topical application of tacrolimus and clotrimazole in the treatment of pityriasis versicolor: A single blind, randomised clinical trial.
==========================================================
Mycoses. 2017 May;60(5):338-342. doi: 10.1111/myc.12598. Epub 2017 Jan 25.
Sepaskhah M1, Sadat MS1, Pakshir K2, Bagheri Z3.
Author information
1
Molecular Dermatology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
2
Basic Sciences in Infectious Diseases Research Center, Department of Parasitology and Mycology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
3
Department of Biostatistics, Faculty of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
Abstract
BACKGROUND:
Pityriasis versicolor (PV) is a common superficial fungal disease. Possibility of emergence of resistant strains to azoles, and difficulty in differentiation of hypopigmented PV and early vitiligo, encouraged us to evaluate the efficacy of topical tacrolimus (a calcineurin inhibitor agent with proven in vitro anti-Malassezia effect) for PV treatment generally and its effect on PV-induced hypopigmentation specifically.
OBJECTIVES:
To evaluate the efficacy of topical tacrolimus on pityriasis versicolor.
PATIENTS/METHODS:
Fifty PV patients were randomly allocated into two equal groups applying either topical clotrimazol or tacrolimus twice daily for 3 weeks. They were evaluated at the beginning of study, in the third and fifth weeks clinically and mycologically (direct smear).
RESULTS:
Although both treatments resulted in global, clinical, and mycological cure of PV, there was no significant difference regarding the mentioned aspects of cure between tacrolimus and clotrimazole treated patients. (P-value: .63, .45, and .26, respectively) Tacrolimus had no significant effect on hypopigmentation in the fifth week follow-up. (P-value: .62).
CONCLUSIONS:
In spite of the lack of efficacy of tacrolimus on PV-induced hypopigmentation, the therapeutic effect on PV introduces tacrolimus as a therapeutic option for PV, especially when early vitiligo is among the differential diagnoses without concerning the aggravating effect of topical corticosteroids on PV.
==========================================================
4.) Comparative clinical trial: fluconazole alone or associated with topical ketoconazole in the treatment of pityriasis versicolor.
==========================================================
Tunis Med. 2016 Feb;94(2):107-11.
Badri T, Hammami H, Bzioueche N, Zouari B, Mokhtar I.
Abstract
BACKGROUND:
The efficacy of ketoconazole and fluconazole in pityriasis versicolor had been proved.
AIM:
To compare the efficacy and the safety of two doses of fluconazole given 1 week apart alone or associated to ketoconazole shampoo.
METHODS:
Our study included all patients with pityriasis versicolor who attended in dermatology department of Habib Thameur Hospital, Tunis (over a 21-month period). During the considered period, patients were randomly assigned in two study groups: G1 receiving fluconazole two doses 300mg given 1 week apart with G2 taken an association of fluconazole (two doses 300mg given 1 week apart) and ketoconazole shampoo the first day.
RESULTS:
Seventy one patients were enrolled in our study: 35 in the fluconazole group and 36 in the fluconazole associated to ketoconazole shampoo comparator group. The mean age was 29.1 years [16-70 years]. Concerning the clinical form, 27% had macular lesions, 24% had plaques and 49% had mixed form. Lesions werehyperchromic52%; hypochromic 15% and erythematous 6%. As for main location, 67% had lesions on the neck; 66% on the trunk, 60% on the shoulders. At the end of the study, there was no significant difference in clinical presentation and in improvement rate of pityriasis versicolor between fluconazole and association of fluconazole and ketoconazole shampoo ((p=0.13 at day 14, p=0.57 at day 28 and p=0.2 at day56).
CONCLUSION:
In this study, we have shown that the improvement rate of PV treated with two doses of 300 mg of fluconazole with one week interval was similar to those of an association of one application of ketoconazole shampoo and the same dose of fluconazole.
==========================================================
6.) Comparison between fluconazole and ketoconazole effectivity in the treatment of pityriasis versicolor.
==========================================================
Mycoses. 2007 Jul;50(4):311-3.
Yazdanpanah MJ1, Azizi H, Suizi B.
Author information
1
Department of Dermatology, Ghaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran. m-yazdanpanah@mums.ac.ir
Abstract
Topical drugs are often effective in limited lesions of pityriasis versicolor; but in extensive cases, systemic drugs are more suitable. Previous studies have shown that ketoconazole and fluconazole are effective in 42-97% and 74-100% of lesions respectively. Our purpose was to compare the effectiveness of a single dose of 400 mg ketoconazole with two doses of 300 mg of fluconazole with 2 weeks interval. Ninety patients with extensive pityriasis versicolor (body involved area > or =25%) were randomly assigned to treatment with either a single dose of 400 mg of ketoconazole or with two doses of 300 mg of fluconazole with 2 weeks interval. One month after the treatment, the improvement rate and side effects were evaluated by clinical examination and questionnaire. Sixty cases (66.7%) completed the study. They were 51 males and nine females, with a mean age of 30 years. At the follow-up visit (1 month after the end of treatment), the improvement rate for ketoconazole (87.9%) was not significantly different from fluconazole (81.5%), (Fisher test: P = 0.37). Due to the hepatotoxicity of ketoconazole, fluconazole appears to be more suitable in the treatment of extensive pityriasis versicolor.
==========================================================
7.) Treatment of pityriasis versicolor with topical application of essential oil of Cymbopogon citratus (DC) Stapf - therapeutic pilot study.
==========================================================
An Bras Dermatol. 2013 May-Jun;88(3):381-5. doi: 10.1590/abd1806-4841.20131800.
Carmo ES1, Pereira Fde O, Cavalcante NM, Gayoso CW, Lima Ede O.
Author information
1
Federal University of Campina Grande (UFCG) - Cuité (PB), Brazil. egbertosantos@ufcg.edu.br
Abstract
BACKGROUND:
Pityriasis versicolor is a fungal infection caused by Malassezia spp. that has frequent relapses.
OBJECTIVES:
The main objective of this research was to perform phase I and II clinical studies, using formulations containing essential oil of Cymbopogon citratus in patients with pityriasis versicolor.
METHODS:
Phase I study included twenty volunteers to ascertain the safety of the formulations. In phase II, 47 volunteers randomly received essential oil formulations at 1.25 μL/mL concentration, for forty days. The shampoo should be applied three times a week and the cream twice a day. A control group in phase II, consisting of 29 volunteers, received the same formulations but with 2% ketoconazole as the active ingredient.
RESULTS:
No significant adverse events were observed in volunteers during Phase I. In Phase II, 30 (63.83%) volunteers using essential oil and 18 (62.07%) using ketoconazole remained until the end of the study. We observed a predominance of lesions in disseminated form, with M. sympodialis detected as the predominant agent identified in cultures. After 40 days of treatment, the rate of mycological cure was 60% (p <0.05) for the group treated with essential oil of C. citratus and over 80% (p <0.05) for the group treated with ketoconazole formulations.
CONCLUSIONS:
Notwithstanding the safety and antifungal effects observed in this study after application of formulations containing the essential oil of C. citratus, further studies with larger populations should be performed to confirm the actual potential of these formulations in the treatment of patients with Pityriasis versicolor.
==========================================================
8.) Atrophying pityriasis versicolor as an idiosyncratic T cell-mediated response to Malassezia: A case series.
=========================================================
J Am Acad Dermatol. 2017 Apr;76(4):730-735. doi: 10.1016/j.jaad.2016.08.062. Epub 2016 Nov 2.
Levy JM1, Magro C2.
Author information
1
University of Alberta, Edmonton, Canada.
2
Weill Cornell Medical College, Manhattan, New York. Electronic address: cym2003@med.cornell.edu.
Abstract
BACKGROUND:
Atrophying pityriasis versicolor (PV), first described in 1971, is a rare variant in which lesions appear atrophic.
OBJECTIVE:
We sought to determine the pathophysiology of atrophying PV.
METHODS:
A retrospective chart review identified 6 cases of atrophying PV. In all cases, routine light microscopy, an elastic tissue stain, and immunohistochemical assessment for the expression of CD3, CD4, CD8, GATA3 and CXCR3 was performed.
RESULTS:
All cases demonstrated hyperkeratosis with intracorneal infiltration by pathogenic hyphal forms as well as epidermal attenuation and papillary dermal elastolysis. A supervening, mild-to-moderate, superficial lymphocytic infiltrate was noted and characterized by a focal CD8+ T cell-mediated interface dermatitis along with a mixed T-cell infiltrate composed of GATA3+ and CXCR3+ T cells.
LIMITATIONS:
Small sample size and the loss of some patients to follow-up.
CONCLUSION:
Atrophying PV represents the sequelae of a mixed helper T-cell (TH1 and TH2) idiosyncratic immune response to Malassezia and can present as a protracted dermatosis that may clinically mimic an atypical lymphocytic infiltrate. TH1 cytokines can recruit histiocytes, a source of elastases, and upregulate matrix metalloproteinase activity, which may contribute to epidermal atrophy.
======================================================
9.) Progress in Malassezia Research in Korea.
=======================================================
Ann Dermatol. 2015 Dec;27(6):647-57. doi: 10.5021/ad.2015.27.6.647. Epub 2015 Dec 7.
Kim SY1, Lee YW1, Choe YB1, Ahn KJ1.
Author information
1
Department of Dermatology, Konkuk University School of Medicine, Seoul, Korea.
Abstract
Yeasts of the genus Malassezia are part of the normal flora of human skin. However, they are also associated with various skin diseases. Since the introduction of Malassezia to the Korean Dermatologic Society two decades ago, remarkable progress has been made in our knowledge of this genus. In this paper, we review recent developments in Malassezia research, including taxonomy and methods for species identification, recent genome analyses, Malassezia species distribution in healthy conditions and in specific skin diseases, trials investigating the mechanisms underlying Malassezia-related diseases, as well as therapeutic options. This review will enhance our understanding of Malassezia yeasts and related skin diseases in Korea.
======================================================
10.) Malassezia species in healthy skin and in dermatological conditions.
======================================================
Int J Dermatol. 2016 May;55(5):494-504. doi: 10.1111/ijd.13116. Epub 2015 Dec 29.
Prohic A1, Jovovic Sadikovic T1, Krupalija-Fazlic M1, Kuskunovic-Vlahovljak S2.
Author information
1
Department of Dermatovenereology, University Clinical Center of Sarajevo, Sarajevo, Bosnia and Herzegovina.
2
Institute of Pathology, Faculty of Medicine, University of Sarajevo, Sarajevo, Bosnia and Herzegovina.
Abstract
The genus Malassezia comprises lipophilic species, the natural habitat of which is the skin of humans and other warm-blooded animals. However, these species have been associated with a diversity of dermatological disorders and even systemic infections. Pityriasis versicolor is the only cutaneous disease etiologically connected to Malassezia yeasts. In the other dermatoses, such as Malassezia folliculitis, seborrheic dermatitis, atopic dermatitis, and psoriasis, these yeasts have been suggested to play pathogenic roles either as direct agents of infection or as trigger factors because there is no evidence that the organisms invade the skin. Malassezia yeasts have been classified into at least 14 species, of which eight have been isolated from human skin, including Malassezia furfur, Malassezia pachydermatis, Malassezia sympodialis, Malassezia slooffiae, Malassezia globosa, Malassezia obtusa, Malassezia restricta, Malassezia dermatis, Malassezia japonica, and Malassezia yamatoensis. Distributions of Malassezia species in the healthy body and in skin diseases have been investigated using culture-based and molecular techniques, and variable results have been reported from different geographical regions. This article reviews and discusses the latest available data on the pathogenicity of Malassezia spp., their distributions in dermatological conditions and in healthy skin, discrepancies in the two methods of identification, and the susceptibility of Malassezia spp. to antifungals.
======================================================
11.) Targeting Malassezia species for novel synthetic and natural antidandruff agents.
======================================================
Curr Med Chem. 2017 Apr 4. doi: 10.2174/0929867324666170404110631. [Epub ahead of print]
Angiolella L1, Carradori S2, Maccallini C3, Giusiano G4, Supuran CT5.
Author information
1
Department of Public Health and Infectious Diseases, Sapienza University of Rome, P.le A. Moro 5, 00185 Rome. Italy.
2
Department of Pharmacy, "G. d`Annunzio" University of Chieti-Pescara, Via dei Vestini 31, 66100 Chieti. Italy.
3
Department of Pharmacy, "G. d'Annunzio" University of Chieti-Pescara, Via dei Vestini 31, 66100 Chieti. Italy.
4
Departamento de Micología, Instituto de Medicina Regional, Facultad de Medicina, Universidad Nacional del Nordeste, CONICET, Resistencia. Argentina.
5
Neurofarba Dept., Section of Pharmaceutical and Nutriceutical Sciences, Università degli Studi di Firenze, Via U. Schiff 6, 50019 Sesto Fiorentino (Florence). Italy.
Abstract
Malassezia spp. are lipophilic yeasts not only present in the normal skin microflora, but also responsible of skin-related diseases (pityriasis versicolor, seborrheic/atopic dermatitis and dandruff) as well as systemic fungal infections in humans and animals. Their treatment and eradication are mainly based on old azole drugs, which are characterized by poor compliance, unpredictable clinical efficacy, emerging resistance and several side effects. These drawbacks have prompted the research toward novel synthetic and natural derivatives/nanomaterials targeting other pivotal enzymes/pathways such as carbonic anhydrase (MgCA) and lipases, alone or in combination, in order to improve the eradication rate of this fungus. This review accomplished an update on this important topic dealing with the latest discoveries of synthetic scaffolds and natural products for the treatment of Malassezia spp.-related diseases, thus suggesting new opportunities to design innovative and alternative anti-dandruff drugs.
======================================================
12.) Biofilm, adherence, and hydrophobicity as virulence factors in Malassezia furfur.
======================================================
Med Mycol. 2017 Mar 9. doi: 10.1093/mmy/myx014. [Epub ahead of print]
Angiolella L1, Leone C1, Rojas F2, Mussin J2, de Los Angeles Sosa M2, Giusiano G3.
Author information
1
Department of Public Health and Infectious Diseases. University of Rome "Sapienza", Italy. Piazzale Aldo Moro 5, 00100 Roma, Italy.
2
Departamento de Micología, Instituto de Medicina Regional, Universidad Nacional del Nordeste, Resistencia, Argentina.
3
Departamento de Micología, Instituto de Medicina Regional, Facultad de Medicina, Universidad Nacional del Nordeste, CONICET, Resistencia, Argentina.
Abstract
Malassezia species are natural inhabitants of the healthy skin. However, under certain conditions, they may cause or exacerbate several skin diseases. The ability of this fungus to colonize or infect is determined by complex interactions between the fungal cell and its virulence factors. This study aims to evaluate "in vitro" the hydrophobicity levels, the adherence on a plastic surface and the biofilm formation of 16 clinical isolates of Malassezia furfur. Cellular surface hydrophobicity (CSH) levels were determined by two-phase system. The biofilm formation was determined by tetrazolium salt (XTT) reduction assay and by Scanning Electron Microscopy (SEM). Results showed many isolates were hydrophobic, adherent, and producers of biofilm on abiotic surfaces with different capacity. SEM observations confirmed an abundant extracellular matrix after 48 h of biofilm formation. About 63% of strains with high production of biofilm showed medium to high percentage of hydrophobicity and/or adherence. In addition, it has been demonstrated a correlation between hydrophobicity, adherence, and biofilm formation in about 60% of strains examined. These important virulence factors could be responsible of this yeast changing from a commensal to a pathogenic status.
======================================================
13.) Antifungal susceptibility testing of Malassezia spp. with an optimized colorimetric broth microdilution method.
======================================================
J Clin Microbiol. 2017 Apr 5. pii: JCM.00338-17. doi: 10.1128/JCM.00338-17. [Epub ahead of print]
Leong C1, Buttafuoco A1, Glatz M2, Bosshard PP2.
Author information
Abstract
Malassezia is a genus of lipid dependent yeasts. It is associated with common skin diseases such as pityriasis versicolor or atopic dermatitis and can cause systemic infections in immunocompromised individuals. Owing to slow growth and lipid requirements of these fastidious yeasts, convenient and reliable antifungal drug susceptibility testing assays for Malassezia spp. are not widely available. We have therefore optimized a broth microdilution assay for the testing of Malassezia that is based on the assays from CLSI and EUCAST for Candida and other yeasts. The addition of ingredients such as lipids and esculin provided a broth medium formulation, which enabled the growth of all Malassezia spp. and could be read with the colorimetric indicator resazurin by visual and by fluorescence reading. We have tested the susceptibility of 52 strains of 13 species of Malassezia against 11 commonly used antifungals. MIC values determined by visual reading were in good agreement with MIC values determined by fluorescence reading. The lowest MICs were found for the azoles itraconazole, posaconazole and voriconazole with MIC90 values of 0.03-1.0 μg/ml, 0.06-0.5 μg/ml and 0.03-2.0 μg/ml, respectively. All Malassezia spp. were resistant to echinocandins and griseofulvin. Some Malassezia spp. also showed high MIC values for ketoconazole, which is the most widely recommended topical antifungal to treat Malassezia skin infections. In summary, our assay enables the fast and reliable susceptibility testing of Malassezia spp. against a large panel of different antifungals.
======================================================
14.) Pityriasis versicolor: an update on pharmacological treatment options.
======================================================
Expert Opin Pharmacother. 2014 Aug;15(12):1707-13. doi: 10.1517/14656566.2014.931373. Epub 2014 Jul 3.
Gupta AK1, Lyons DC.
Author information
1
University of Toronto, Department of Medicine , Toronto , Canada.
Abstract
INTRODUCTION:
Pityriasis versicolor (PV) is a superficial fungal infection caused by Malassezia species; a yeast that naturally colonizes on the skins surface. High efficacy rates are generally obtained with both topical and systemic treatments. However, recurrence rates following successful treatment remain high and there are no dosage guidelines available for administration of systemic antifungal agents that carry risks of adverse events.
AREAS COVERED:
This review focused on providing an overview of existing treatments for PV and an introduction to new treatments. A literature search was conducted using the search strategy, pityriasis versicolor OR tinea versicolor. Over the past decade, few new treatments have been introduced, but the efficacy and the dosing regimens of existing treatments have been systematically reviewed. The results of these reviews are discussed.
EXPERT OPINION:
Existing topical and systemic agents are both effective treatments against PV. Previous dosage recommendations for systemic agents have been modified based on recent evidence elucidated in systematic reviews. However, the absence of standardized collection and reporting practices in clinical trials precludes any conclusions to be drawn regarding the efficacy and safety of topical and systemic agents in comparison or in concert with each other.
===========================================================
15.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
===========================================================
Acta Derm Venereol Suppl (Stockh). 1979;(86):1-23.
Faergemann J.
Abstract
In patients with tinea versicolor, Pityrosporum orbiculare was cultured from tinea versicolor lesions in 100%, from normal-looking skin in 80%, and from apparently healed lesions in 69%. P. orbiculare was isolated from normal skin in 85% of patients with seborrheic dermatitis and in 90% of volunteers. The best substrate for isolation of P. orbiculare was a peptone-glucose-yeast extract medium containing glycerol monostearate and Tween 80, overlaid with olive oil. Germ tubes were produced when P. orbiculare was incubated in an atmosphere containing air with 7% CO2. Cultures of P. orbiculare and P. ovale did not show any fluorescence in Wood's light. The in vitro activity of miconazole, clotrimazole, econazole, sodium omadine, and sodium thiosulphate against P. orbiculare was found to correlate to the good clinical effect of these drugs in tinea versicolor. In addition several substances used as solvents or in vehicles had an inhibitory activity against P. orbiculare in vitro. Inoculation with P. orbiculare under plastic occlusion on the glabrous follicle-rich inside of the rabbit ear resulted in a tinea versicolor-like lesion after I week in 3 of 4 animals. One week after inoculation with P. orbiculare under plastic occlusion, experimental infections similar to those found clinically in tinea versicolor were seen in 10 of 12 patients with a history of tinea versicolor and in 3 of 6 normal volunteers. It was not possible to produce experimental infections without occlusion. Spontaneous healing usually occurred. In a retrospective study of 232 patients and prospective survey of 48 patients regarding susceptibility factors in tinea versicolor a higher (10.4%) than expected (3.8%) connection to seborrheic dermatitis was found.
===========================================================
16.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
===========================================================
Acta Derm Venereol Suppl (Stockh). 1979;(86):1-23.
Faergemann J.
Abstract
In patients with tinea versicolor, Pityrosporum orbiculare was cultured from tinea versicolor lesions in 100%, from normal-looking skin in 80%, and from apparently healed lesions in 69%. P. orbiculare was isolated from normal skin in 85% of patients with seborrheic dermatitis and in 90% of volunteers. The best substrate for isolation of P. orbiculare was a peptone-glucose-yeast extract medium containing glycerol monostearate and Tween 80, overlaid with olive oil. Germ tubes were produced when P. orbiculare was incubated in an atmosphere containing air with 7% CO2. Cultures of P. orbiculare and P. ovale did not show any fluorescence in Wood's light. The in vitro activity of miconazole, clotrimazole, econazole, sodium omadine, and sodium thiosulphate against P. orbiculare was found to correlate to the good clinical effect of these drugs in tinea versicolor. In addition several substances used as solvents or in vehicles had an inhibitory activity against P. orbiculare in vitro. Inoculation with P. orbiculare under plastic occlusion on the glabrous follicle-rich inside of the rabbit ear resulted in a tinea versicolor-like lesion after I week in 3 of 4 animals. One week after inoculation with P. orbiculare under plastic occlusion, experimental infections similar to those found clinically in tinea versicolor were seen in 10 of 12 patients with a history of tinea versicolor and in 3 of 6 normal volunteers. It was not possible to produce experimental infections without occlusion. Spontaneous healing usually occurred. In a retrospective study of 232 patients and prospective survey of 48 patients regarding susceptibility factors in tinea versicolor a higher (10.4%) than expected (3.8%) connection to seborrheic dermatitis was found.
===========================================================
17.) Mycological Considerations in the Topical Treatment of Superficial Fungal Infections.
===========================================================
J Drugs Dermatol. 2016 Feb;15(2 Suppl):s49-55.
Rosen T.
Abstract
Trichophyton rubrum remains the most common pathogenic dermatophyte in the United States, Europe, and industrialized Asia, although other species are predminant elsewhere. Candida albicans is the most common pathogenic yeast, with other species occasionally encountered. Just a few of the 14 described species of Malassezia cause pityriasis versicolor worldwide. FDA approval does not always accurately reflect the potential utility of any given topical antifungal agent. Azole, hydroxypyridone, and allylamine agents are beneficial in the management of dermatophytosis; however, the allylamines may lead to faster symptom resolution and a higher degree of sustained response. Although in actual clinical use the allylamines have all shown some activity against superficial cutaneous candidiasis and pityriasis versicolor, the azole agents remain drugs of choice. Ciclopirox is an excellent broad-spectrum antifungal agent. Optimal topical therapy for superficial fungal infections cannot yet be reliably based upon in-vitro laboratory determination of sensitivity. Inherent antibacterial and anti-inflammatory properties possessed by some antifungal agents may be exploited for clinical purposes. Candida species may be azole-insensitive due to efflux pumps or an altered target enzyme. So-called "antifungal resistance" of dermatophyets is actually due to poor patient adherence (either in dosing or treatment duration), or to reinfection.
===========================================================
18.) Single-dose fluconazole versus itraconazole in pityriasis versicolor.
===========================================================
Dermatology. 2004;208(1):55-9.
Partap R1, Kaur I, Chakrabarti A, Kumar B.
Author information
1
Department of Dermatology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Abstract
BACKGROUND:
The new antifungal triazoles itraconazole and fluconazole have revolutionized the treatment of pityriasis versicolor. Both drugs have shown promising results in different dose schedules.
OBJECTIVE:
To compare the efficacy and safety of single oral dose treatment with fluconazole versus itraconazole in patients with pityriasis versicolor.
METHODS:
A total of 40 patients with pityriasis versicolor were allocated randomly to group A and group B. A single dose of fluconazole (400 mg) or itraconazole (400 mg) was given orally to group A or group B patients, respectively. Patients were assessed mycologically by KOH and culture. Culture was done from lesional and perilesional skin to quantify growth and to observe the effect of these drugs and the persistence/reappearance of the fungus in relation to relapse at 2 and 8 weeks. Relapse was defined as reappearance or worsening of clinical signs and symptoms or positive KOH/culture after initial improvement.
RESULTS:
Thirteen (65%) patients in the fluconazole group and 4 (20%) patients in the itraconazole group became culture negative at the end of 8 weeks. Relapse was found to be higher in the itraconazole group compared to the fluconazole group (60 vs. 35%). A direct correlation was found between the relapse rate and positivity of perilesional skin for Malassezia furfur.
CONCLUSION:
In the same dosing, fluconazole was found to be more effective than itraconazole; however, both drugs were found to be safe.
===========================================================
19.) Itraconazole in tinea versicolor: a review.
===========================================================
J Am Acad Dermatol. 1990 Sep;23(3 Pt 2):551-4.
Delescluse J1.
Author information
1
Department of Dermatology, Clinic Cesar De Paepe, Brussels, Belgium.
Abstract
Itraconazole, a new orally active triazole antifungal, has been tested in patients with pityriasis versicolor. A number of studies have shown that itraconazole is effective for this mild fungal skin disease. The total dose required for effective treatment is 1000 mg, and it has been given as 200 mg for 5 days or 7 days. The organisms disappear slowly from the skin, even when dead, and the results should be assessed clinically and mycologically at around 3 to 4 weeks after treatment. Numerous studies have shown that itraconazole is superior to placebo and as effective as selenium sulfide, clotrimazole, and ciclopirox olamine. It is also better tolerated by patients than selenium sulfide.
===========================================================
20.) [Cutaneous Malassezia infections and Malassezia associated dermatoses: An update].
===========================================================
Hautarzt. 2015 Jun;66(6):465-84; quiz 485-6. doi: 10.1007/s00105-015-3631-z.
[Article in German]
Nenoff P1, Krüger C, Mayser P.
Author information
1
Labor für medizinische Mikrobiologie, Partnerschaft Prof. Dr. med. Pietro Nenoff & Dr. med. Constanze Krüger, Straße des Friedens 8, 04579, Mölbis, Deutschland, nenoff@mykologie-experten.de.
Abstract
The lipophilic yeast fungus Malassezia (M.) spp. is the only fungal genus or species which is part of the physiological human microbiome. Today, at least 14 different Malassezia species are known; most of them can only be identified using molecular biological techniques. As a facultative pathogenic microorganism, Malassezia represents the causative agent both of superficial cutaneous infections and of blood stream infections. Pityriasis versicolor is the probably most frequent infection caused by Malassezia. Less common, Malassezia folliculitis occurs. There is only an episodic report on Malassezia-induced onychomycosis. Seborrhoeic dermatitis represents a Malassezia-associated inflammatory dermatosis. In addition, Malassezia allergenes should be considered as the trigger of "Head-Neck"-type atopic dermatitis. Ketoconazole possesses the strongest in vitro activity against Malassezia, and represents the treatment of choice for topical therapy of pityriasis versicolor. Alternatives include other azole antifungals but also the allylamine terbinafine and the hydroxypyridone antifungal agent ciclopirox olamine. "Antiseborrhoeic" agents, e.g. zinc pyrithione, selenium disulfide, and salicylic acid, are also effective in pityriasis versicolor. The drug of choice for oral treatment of pityriasis versicolor is itraconazole; an effective alternative represents fluconazole. Seborrhoeic dermatitis is best treated with topical medication, including topical corticosteroids and antifungal agents like ketoconazole or sertaconazole. Calcineurin inhibitors, e.g. pimecrolimus and tacrolimus, are reliable in seborrhoeic dermatitis, however are used off-label.
===========================================================
21.) A double-blind comparative study of sodium sulfacetamide lotion 10% versus selenium sulfide lotion 2.5% in the treatment of pityriasis (tinea) versicolor.
============================================================
Cutis. 2004 Jun;73(6):425-9.
Hull CA1, Johnson SM.
Author information
1
Department of Dermatology, University of Arkansas for Medical Sciences, Little Rock, AR 72205, USA.
Abstract
Pityriasis (tinea) versicolor, which consists of hyperpigmented and hypopigmented scaly patches, is often difficult to treat. A double-blind comparative study between once-a-day sodium sulfacetamide lotion and selenium sulfide lotion was undertaken. Both treatments were safe and efficacious. Selenium sulfide was statistically more efficacious (76.2% vs 47.8%, P=.013).
===========================================================
22.) Selenium sulfide in tinea versicolor: blood and urine levels.
===========================================================
J Am Acad Dermatol. 1984 Aug;11(2 Pt 1):238-41.
Sánchez JL, Torres VM.
Abstract
The safety of topical selenium sulfide lotion in man has been demonstrated previously. Twenty male patients with a diagnosis of tinea versicolor were randomly assigned to two parallel groups who applied selenium sulfide lotion or the vehicle to the entire skin surface, excluding mucous membranes, for 10 minutes once daily for 7 consecutive days. Blood and urine selenium levels were determined before and after treatment and showed no significant differences between the active drug and vehicle groups on any study day. It would appear that no significant absorption of selenium took place as a result of this treatment regimen.
===========================================================
23.) New Antifungal Agents and New Formulations Against Dermatophytes.
===========================================================
Mycopathologia. 2017 Feb;182(1-2):127-141. doi: 10.1007/s11046-016-0045-0. Epub 2016 Aug 8.
Gupta AK1,2, Foley KA3, Versteeg SG3.
Author information
1
Department of Medicine, University of Toronto, Toronto, Canada. publications@mediproberesearch.com.
2
Mediprobe Research Inc., 645 Windermere Road, London, ON, Canada. publications@mediproberesearch.com.
3
Mediprobe Research Inc., 645 Windermere Road, London, ON, Canada.
Abstract
A variety of oral and topical antifungal agents are available for the treatment of superficial fungal infections caused by dermatophytes. This review builds on the antifungal therapy update published in this journal for the first special issue on Dermatophytosis (Gupta and Cooper 2008;166:353-67). Since 2008, there have not been additions to the oral antifungal armamentarium, with terbinafine, itraconazole, and fluconazole still in widespread use, albeit for generally more severe or recalcitrant infections. Griseofulvin is used in the treatment of tinea capitis. Oral ketoconazole has fallen out of favor in many jurisdictions due to risks of hepatotoxicity. Topical antifungals, applied once or twice daily, are the primary treatment for tinea pedis, tinea corporis/tinea cruris, and mild cases of tinea unguium. Newer topical antifungal agents introduced include the azoles, efinaconazole, luliconazole, and sertaconazole, and the oxaborole, tavaborole. Research is focused on developing formulations of existing topical antifungals that utilize novel delivery systems in order to enhance treatment efficacy and compliance.
===========================================================
24.) Tavaborole, Efinaconazole, and Luliconazole: Three New Antimycotic Agents for the Treatment of Dermatophytic Fungi.
===========================================================
J Pharm Pract. 2016 Aug 3. pii: 0897190016660487. [Epub ahead of print]
Saunders J1, Maki K1, Koski R2, Nybo SE3.
Author information
1
College of Pharmacy, Ferris State University, Big Rapids, MI, USA.
2
UP Health System Marquette, Marquette, MI, USA.
3
College of Pharmacy, Ferris State University, Big Rapids, MI, USA ericnybo@ferris.edu.
Abstract
Fungal diseases of the nail bed (onychomycosis) and epidermis are recurrent illnesses in the elderly and immunocompromised patients, which have few efficacious treatment options. Current treatment options for onychomycosis are limited to topical agents, laser treatment, and oral antifungals. Previous generations of topical agents were not efficacious, owing to poor penetration of the nail bed. Oral antifungal drugs, such as itraconazole, terbinafine, and fluconazole, not only give better response rates but also inhibit a host of CYP450 enzymes. Oral antifungals can exacerbate drug-drug interactions for patients taking other medications concurrently. Newer topical agents might recognize improved efficacy and provide therapeutic alternatives when the use of oral antifungal agents is contraindicated. Recently, the Food and Drug Administration (FDA) approved efinaconazole and tavaborole for the treatment of onychomycosis. Additionally, the FDA approved luliconazole for the treatment of tinea pedis, tinea cruris, and tinea corporis. This review examines the mechanism of action, spectrum of activity, pharmacokinetics, and clinical trials data and considers the place in therapy for these 3 new antimycotic agents.
===========================================================
25.) Therapeutic efficacy and safety of the new antimycotic sertaconazole in the treatment of Pityriasis versicolor.
===========================================================
Arzneimittelforschung. 1992 May;42(5A):764-7.
Nasarre J1, Umbert P, Herrero E, Roset P, Márquez M, Torres J, Ortiz JA.
Author information
1
Dermatology Department, Hospital Sagrado Corazón, Medical School, University of Barcelona, Spain.
Abstract
The activity of 7-chloro-3-[1-(2,4-dichlorophenyl)-2-(1H-imidazol-1-yl) ethoxy-methyl]benzo[b]thiophene (sertaconazole, FI-7045, CAS 99592-32,2) was studied in a randomized parallel double-blind clinical trial on 21 patients suffering from Pityriasis versicolor (confirmed by KOH microscopic examination and exploration with Wood's light). The patients were divided into two treatment groups: one with 11 patients receiving sertaconazole 1% cream and the other with 10 patients receiving sertaconazole 2% cream. The cream was applied twice a day during 4 weeks. The data were assessed clinically and microscopically (optical and fluorescence). All the patients were cured (100% cure), showing excellent efficacy. A check-up performed after the end of the treatment showed no relapses of infection. The drug safety was optimum, since no local or general undesirable effects were recorded, nor were there any changes in the analytical parameters studied in the 21 patients. Because of its high antifungal activity and excellent safety, sertaconazole represents an important advance in the topical therapy of this disease.
===========================================================
25.) Whole genome sequencing analysis of the cutaneous pathogenic yeast Malassezia restricta and identification of the major lipase expressed on the scalp of patients with dandruff.
===========================================================
Mycoses. 2017 Mar;60(3):188-197. doi: 10.1111/myc.12586. Epub 2016 Nov 24.
Park M1, Cho YJ2, Lee YW3,4, Jung WH1.
Author information
1
Department of Systems Biotechnology, Chung-Ang University, Anseong, Korea.
2
ChunLab, Inc., Seoul National University, Seoul, Korea.
3
Department of Dermatology, School of Medicine, Konkuk University, Seoul, Korea.
4
Research Institute of Medical Science, Konkuk University, Seoul, Korea.
Abstract
Malassezia species are opportunistic pathogenic fungi that are frequently associated with seborrhoeic dermatitis, including dandruff. Most Malassezia species are lipid dependent, a property that is compensated by breaking down host sebum into fatty acids by lipases. In this study, we aimed to sequence and analyse the whole genome of Malassezia restricta KCTC 27527, a clinical isolate from a Korean patient with severe dandruff, to search for lipase orthologues and identify the lipase that is the most frequently expressed on the scalp of patients with dandruff. The genome of M. restricta KCTC 27527 was sequenced using the Illumina MiSeq and PacBio platforms. Lipase orthologues were identified by comparison with known lipase genes in the genomes of Malassezia globosa and Malassezia sympodialis. The expression of the identified lipase genes was directly evaluated in swab samples from the scalps of 56 patients with dandruff. We found that, among the identified lipase-encoding genes, the gene encoding lipase homolog MRES_03670, named LIP5 in this study, was the most frequently expressed lipase in the swab samples. Our study provides an overview of the genome of a clinical isolate of M. restricta and fundamental information for elucidating the role of lipases during fungus-host interaction.
===========================================================
Pan Afr Med J. 2017 Jan 23;26:31. doi: 10.11604/pamj.2017.26.31.11504. eCollection 2017.
[Article in French]
Dioussé P1, Ly F2, Bammo M3, Lizia S2, Diallo TAA1, Dione H1, Sarr F1, Gueye RD1, Gueye AM1, Dieng MT2, Diop BM1, Ka MM1.
Author information
1
UFR des Sciences de la Santé, Université de Thiès, Sénégal.
2
Dermatologie, Université Cheikh Anta Diop, Dakar, Sénégal.
3
Dermatologie, Hôpital Régional de Thiès, Sénégal.
Abstract
We report two cases of Pityriasis versicolor (PV) in infants aged 12 and 18 months. The latter were brought to medical attention because of hypochromic and achromic, round macules involving the limbs and the face. Physical examination of their mothers showed voluntary depigmentation for cosmetic purposes due to the use of corticosteroids and hydroquinone, on average, over a 5-year period. The scotch tape test performed in one of the infants and his mother showed short filaments and clusters of spores. Treatment was based on ketoconazole. After 8 weeks, all patients reported favorable outcomes despite the persistence of some hypochomic macules. The peculiarities of this study are, on the one hand the topography of the lower limbs and on the other hand a positive family history of PV whose occurrence is favored by the use of depigmenting agents based on corticosteroids. Corticosteroids favor the atrophic and achromic feature of the lesions. Indeed, achromic lesions on the lower limbs were described in adults undergoing artificial depigmentation.
==========================================================
2.) Folliculocentric tinea versicolor.
==========================================================
Dermatol Online J. 2017 Feb 15;23(2). pii: 13030/qt5kj574bd.
Hudson A1, Carroll B, Kim SJ.
Author information
1
Department of Dermatology, Texas Tech University Health Sciences Center, Lubbock. andrew.hudson@ttuhsc.edu.
Abstract
Tinea versicolor (TV) is typically an asymptomatic fungal infection of the stratum corneum owing to Malassezia overgrowth. It presents as hypo or hyperpigmented macules with fine scale that coalesce into patches on the trunk, neck, and/or arms. Presented in this report is a 34-year-old man with an interesting case of folliculocentric tinea versicolor manifesting as perifollicular hypopigmented macules on the lower back.
==========================================================
3.) Comparative efficacy of topical application of tacrolimus and clotrimazole in the treatment of pityriasis versicolor: A single blind, randomised clinical trial.
==========================================================
Mycoses. 2017 May;60(5):338-342. doi: 10.1111/myc.12598. Epub 2017 Jan 25.
Sepaskhah M1, Sadat MS1, Pakshir K2, Bagheri Z3.
Author information
1
Molecular Dermatology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
2
Basic Sciences in Infectious Diseases Research Center, Department of Parasitology and Mycology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
3
Department of Biostatistics, Faculty of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
Abstract
BACKGROUND:
Pityriasis versicolor (PV) is a common superficial fungal disease. Possibility of emergence of resistant strains to azoles, and difficulty in differentiation of hypopigmented PV and early vitiligo, encouraged us to evaluate the efficacy of topical tacrolimus (a calcineurin inhibitor agent with proven in vitro anti-Malassezia effect) for PV treatment generally and its effect on PV-induced hypopigmentation specifically.
OBJECTIVES:
To evaluate the efficacy of topical tacrolimus on pityriasis versicolor.
PATIENTS/METHODS:
Fifty PV patients were randomly allocated into two equal groups applying either topical clotrimazol or tacrolimus twice daily for 3 weeks. They were evaluated at the beginning of study, in the third and fifth weeks clinically and mycologically (direct smear).
RESULTS:
Although both treatments resulted in global, clinical, and mycological cure of PV, there was no significant difference regarding the mentioned aspects of cure between tacrolimus and clotrimazole treated patients. (P-value: .63, .45, and .26, respectively) Tacrolimus had no significant effect on hypopigmentation in the fifth week follow-up. (P-value: .62).
CONCLUSIONS:
In spite of the lack of efficacy of tacrolimus on PV-induced hypopigmentation, the therapeutic effect on PV introduces tacrolimus as a therapeutic option for PV, especially when early vitiligo is among the differential diagnoses without concerning the aggravating effect of topical corticosteroids on PV.
==========================================================
4.) Comparative clinical trial: fluconazole alone or associated with topical ketoconazole in the treatment of pityriasis versicolor.
==========================================================
Tunis Med. 2016 Feb;94(2):107-11.
Badri T, Hammami H, Bzioueche N, Zouari B, Mokhtar I.
Abstract
BACKGROUND:
The efficacy of ketoconazole and fluconazole in pityriasis versicolor had been proved.
AIM:
To compare the efficacy and the safety of two doses of fluconazole given 1 week apart alone or associated to ketoconazole shampoo.
METHODS:
Our study included all patients with pityriasis versicolor who attended in dermatology department of Habib Thameur Hospital, Tunis (over a 21-month period). During the considered period, patients were randomly assigned in two study groups: G1 receiving fluconazole two doses 300mg given 1 week apart with G2 taken an association of fluconazole (two doses 300mg given 1 week apart) and ketoconazole shampoo the first day.
RESULTS:
Seventy one patients were enrolled in our study: 35 in the fluconazole group and 36 in the fluconazole associated to ketoconazole shampoo comparator group. The mean age was 29.1 years [16-70 years]. Concerning the clinical form, 27% had macular lesions, 24% had plaques and 49% had mixed form. Lesions werehyperchromic52%; hypochromic 15% and erythematous 6%. As for main location, 67% had lesions on the neck; 66% on the trunk, 60% on the shoulders. At the end of the study, there was no significant difference in clinical presentation and in improvement rate of pityriasis versicolor between fluconazole and association of fluconazole and ketoconazole shampoo ((p=0.13 at day 14, p=0.57 at day 28 and p=0.2 at day56).
CONCLUSION:
In this study, we have shown that the improvement rate of PV treated with two doses of 300 mg of fluconazole with one week interval was similar to those of an association of one application of ketoconazole shampoo and the same dose of fluconazole.
==========================================================
6.) Comparison between fluconazole and ketoconazole effectivity in the treatment of pityriasis versicolor.
==========================================================
Mycoses. 2007 Jul;50(4):311-3.
Yazdanpanah MJ1, Azizi H, Suizi B.
Author information
1
Department of Dermatology, Ghaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran. m-yazdanpanah@mums.ac.ir
Abstract
Topical drugs are often effective in limited lesions of pityriasis versicolor; but in extensive cases, systemic drugs are more suitable. Previous studies have shown that ketoconazole and fluconazole are effective in 42-97% and 74-100% of lesions respectively. Our purpose was to compare the effectiveness of a single dose of 400 mg ketoconazole with two doses of 300 mg of fluconazole with 2 weeks interval. Ninety patients with extensive pityriasis versicolor (body involved area > or =25%) were randomly assigned to treatment with either a single dose of 400 mg of ketoconazole or with two doses of 300 mg of fluconazole with 2 weeks interval. One month after the treatment, the improvement rate and side effects were evaluated by clinical examination and questionnaire. Sixty cases (66.7%) completed the study. They were 51 males and nine females, with a mean age of 30 years. At the follow-up visit (1 month after the end of treatment), the improvement rate for ketoconazole (87.9%) was not significantly different from fluconazole (81.5%), (Fisher test: P = 0.37). Due to the hepatotoxicity of ketoconazole, fluconazole appears to be more suitable in the treatment of extensive pityriasis versicolor.
==========================================================
7.) Treatment of pityriasis versicolor with topical application of essential oil of Cymbopogon citratus (DC) Stapf - therapeutic pilot study.
==========================================================
An Bras Dermatol. 2013 May-Jun;88(3):381-5. doi: 10.1590/abd1806-4841.20131800.
Carmo ES1, Pereira Fde O, Cavalcante NM, Gayoso CW, Lima Ede O.
Author information
1
Federal University of Campina Grande (UFCG) - Cuité (PB), Brazil. egbertosantos@ufcg.edu.br
Abstract
BACKGROUND:
Pityriasis versicolor is a fungal infection caused by Malassezia spp. that has frequent relapses.
OBJECTIVES:
The main objective of this research was to perform phase I and II clinical studies, using formulations containing essential oil of Cymbopogon citratus in patients with pityriasis versicolor.
METHODS:
Phase I study included twenty volunteers to ascertain the safety of the formulations. In phase II, 47 volunteers randomly received essential oil formulations at 1.25 μL/mL concentration, for forty days. The shampoo should be applied three times a week and the cream twice a day. A control group in phase II, consisting of 29 volunteers, received the same formulations but with 2% ketoconazole as the active ingredient.
RESULTS:
No significant adverse events were observed in volunteers during Phase I. In Phase II, 30 (63.83%) volunteers using essential oil and 18 (62.07%) using ketoconazole remained until the end of the study. We observed a predominance of lesions in disseminated form, with M. sympodialis detected as the predominant agent identified in cultures. After 40 days of treatment, the rate of mycological cure was 60% (p <0.05) for the group treated with essential oil of C. citratus and over 80% (p <0.05) for the group treated with ketoconazole formulations.
CONCLUSIONS:
Notwithstanding the safety and antifungal effects observed in this study after application of formulations containing the essential oil of C. citratus, further studies with larger populations should be performed to confirm the actual potential of these formulations in the treatment of patients with Pityriasis versicolor.
==========================================================
8.) Atrophying pityriasis versicolor as an idiosyncratic T cell-mediated response to Malassezia: A case series.
=========================================================
J Am Acad Dermatol. 2017 Apr;76(4):730-735. doi: 10.1016/j.jaad.2016.08.062. Epub 2016 Nov 2.
Levy JM1, Magro C2.
Author information
1
University of Alberta, Edmonton, Canada.
2
Weill Cornell Medical College, Manhattan, New York. Electronic address: cym2003@med.cornell.edu.
Abstract
BACKGROUND:
Atrophying pityriasis versicolor (PV), first described in 1971, is a rare variant in which lesions appear atrophic.
OBJECTIVE:
We sought to determine the pathophysiology of atrophying PV.
METHODS:
A retrospective chart review identified 6 cases of atrophying PV. In all cases, routine light microscopy, an elastic tissue stain, and immunohistochemical assessment for the expression of CD3, CD4, CD8, GATA3 and CXCR3 was performed.
RESULTS:
All cases demonstrated hyperkeratosis with intracorneal infiltration by pathogenic hyphal forms as well as epidermal attenuation and papillary dermal elastolysis. A supervening, mild-to-moderate, superficial lymphocytic infiltrate was noted and characterized by a focal CD8+ T cell-mediated interface dermatitis along with a mixed T-cell infiltrate composed of GATA3+ and CXCR3+ T cells.
LIMITATIONS:
Small sample size and the loss of some patients to follow-up.
CONCLUSION:
Atrophying PV represents the sequelae of a mixed helper T-cell (TH1 and TH2) idiosyncratic immune response to Malassezia and can present as a protracted dermatosis that may clinically mimic an atypical lymphocytic infiltrate. TH1 cytokines can recruit histiocytes, a source of elastases, and upregulate matrix metalloproteinase activity, which may contribute to epidermal atrophy.
======================================================
9.) Progress in Malassezia Research in Korea.
=======================================================
Ann Dermatol. 2015 Dec;27(6):647-57. doi: 10.5021/ad.2015.27.6.647. Epub 2015 Dec 7.
Kim SY1, Lee YW1, Choe YB1, Ahn KJ1.
Author information
1
Department of Dermatology, Konkuk University School of Medicine, Seoul, Korea.
Abstract
Yeasts of the genus Malassezia are part of the normal flora of human skin. However, they are also associated with various skin diseases. Since the introduction of Malassezia to the Korean Dermatologic Society two decades ago, remarkable progress has been made in our knowledge of this genus. In this paper, we review recent developments in Malassezia research, including taxonomy and methods for species identification, recent genome analyses, Malassezia species distribution in healthy conditions and in specific skin diseases, trials investigating the mechanisms underlying Malassezia-related diseases, as well as therapeutic options. This review will enhance our understanding of Malassezia yeasts and related skin diseases in Korea.
======================================================
10.) Malassezia species in healthy skin and in dermatological conditions.
======================================================
Int J Dermatol. 2016 May;55(5):494-504. doi: 10.1111/ijd.13116. Epub 2015 Dec 29.
Prohic A1, Jovovic Sadikovic T1, Krupalija-Fazlic M1, Kuskunovic-Vlahovljak S2.
Author information
1
Department of Dermatovenereology, University Clinical Center of Sarajevo, Sarajevo, Bosnia and Herzegovina.
2
Institute of Pathology, Faculty of Medicine, University of Sarajevo, Sarajevo, Bosnia and Herzegovina.
Abstract
The genus Malassezia comprises lipophilic species, the natural habitat of which is the skin of humans and other warm-blooded animals. However, these species have been associated with a diversity of dermatological disorders and even systemic infections. Pityriasis versicolor is the only cutaneous disease etiologically connected to Malassezia yeasts. In the other dermatoses, such as Malassezia folliculitis, seborrheic dermatitis, atopic dermatitis, and psoriasis, these yeasts have been suggested to play pathogenic roles either as direct agents of infection or as trigger factors because there is no evidence that the organisms invade the skin. Malassezia yeasts have been classified into at least 14 species, of which eight have been isolated from human skin, including Malassezia furfur, Malassezia pachydermatis, Malassezia sympodialis, Malassezia slooffiae, Malassezia globosa, Malassezia obtusa, Malassezia restricta, Malassezia dermatis, Malassezia japonica, and Malassezia yamatoensis. Distributions of Malassezia species in the healthy body and in skin diseases have been investigated using culture-based and molecular techniques, and variable results have been reported from different geographical regions. This article reviews and discusses the latest available data on the pathogenicity of Malassezia spp., their distributions in dermatological conditions and in healthy skin, discrepancies in the two methods of identification, and the susceptibility of Malassezia spp. to antifungals.
======================================================
11.) Targeting Malassezia species for novel synthetic and natural antidandruff agents.
======================================================
Curr Med Chem. 2017 Apr 4. doi: 10.2174/0929867324666170404110631. [Epub ahead of print]
Angiolella L1, Carradori S2, Maccallini C3, Giusiano G4, Supuran CT5.
Author information
1
Department of Public Health and Infectious Diseases, Sapienza University of Rome, P.le A. Moro 5, 00185 Rome. Italy.
2
Department of Pharmacy, "G. d`Annunzio" University of Chieti-Pescara, Via dei Vestini 31, 66100 Chieti. Italy.
3
Department of Pharmacy, "G. d'Annunzio" University of Chieti-Pescara, Via dei Vestini 31, 66100 Chieti. Italy.
4
Departamento de Micología, Instituto de Medicina Regional, Facultad de Medicina, Universidad Nacional del Nordeste, CONICET, Resistencia. Argentina.
5
Neurofarba Dept., Section of Pharmaceutical and Nutriceutical Sciences, Università degli Studi di Firenze, Via U. Schiff 6, 50019 Sesto Fiorentino (Florence). Italy.
Abstract
Malassezia spp. are lipophilic yeasts not only present in the normal skin microflora, but also responsible of skin-related diseases (pityriasis versicolor, seborrheic/atopic dermatitis and dandruff) as well as systemic fungal infections in humans and animals. Their treatment and eradication are mainly based on old azole drugs, which are characterized by poor compliance, unpredictable clinical efficacy, emerging resistance and several side effects. These drawbacks have prompted the research toward novel synthetic and natural derivatives/nanomaterials targeting other pivotal enzymes/pathways such as carbonic anhydrase (MgCA) and lipases, alone or in combination, in order to improve the eradication rate of this fungus. This review accomplished an update on this important topic dealing with the latest discoveries of synthetic scaffolds and natural products for the treatment of Malassezia spp.-related diseases, thus suggesting new opportunities to design innovative and alternative anti-dandruff drugs.
======================================================
12.) Biofilm, adherence, and hydrophobicity as virulence factors in Malassezia furfur.
======================================================
Med Mycol. 2017 Mar 9. doi: 10.1093/mmy/myx014. [Epub ahead of print]
Angiolella L1, Leone C1, Rojas F2, Mussin J2, de Los Angeles Sosa M2, Giusiano G3.
Author information
1
Department of Public Health and Infectious Diseases. University of Rome "Sapienza", Italy. Piazzale Aldo Moro 5, 00100 Roma, Italy.
2
Departamento de Micología, Instituto de Medicina Regional, Universidad Nacional del Nordeste, Resistencia, Argentina.
3
Departamento de Micología, Instituto de Medicina Regional, Facultad de Medicina, Universidad Nacional del Nordeste, CONICET, Resistencia, Argentina.
Abstract
Malassezia species are natural inhabitants of the healthy skin. However, under certain conditions, they may cause or exacerbate several skin diseases. The ability of this fungus to colonize or infect is determined by complex interactions between the fungal cell and its virulence factors. This study aims to evaluate "in vitro" the hydrophobicity levels, the adherence on a plastic surface and the biofilm formation of 16 clinical isolates of Malassezia furfur. Cellular surface hydrophobicity (CSH) levels were determined by two-phase system. The biofilm formation was determined by tetrazolium salt (XTT) reduction assay and by Scanning Electron Microscopy (SEM). Results showed many isolates were hydrophobic, adherent, and producers of biofilm on abiotic surfaces with different capacity. SEM observations confirmed an abundant extracellular matrix after 48 h of biofilm formation. About 63% of strains with high production of biofilm showed medium to high percentage of hydrophobicity and/or adherence. In addition, it has been demonstrated a correlation between hydrophobicity, adherence, and biofilm formation in about 60% of strains examined. These important virulence factors could be responsible of this yeast changing from a commensal to a pathogenic status.
======================================================
13.) Antifungal susceptibility testing of Malassezia spp. with an optimized colorimetric broth microdilution method.
======================================================
J Clin Microbiol. 2017 Apr 5. pii: JCM.00338-17. doi: 10.1128/JCM.00338-17. [Epub ahead of print]
Leong C1, Buttafuoco A1, Glatz M2, Bosshard PP2.
Author information
Abstract
Malassezia is a genus of lipid dependent yeasts. It is associated with common skin diseases such as pityriasis versicolor or atopic dermatitis and can cause systemic infections in immunocompromised individuals. Owing to slow growth and lipid requirements of these fastidious yeasts, convenient and reliable antifungal drug susceptibility testing assays for Malassezia spp. are not widely available. We have therefore optimized a broth microdilution assay for the testing of Malassezia that is based on the assays from CLSI and EUCAST for Candida and other yeasts. The addition of ingredients such as lipids and esculin provided a broth medium formulation, which enabled the growth of all Malassezia spp. and could be read with the colorimetric indicator resazurin by visual and by fluorescence reading. We have tested the susceptibility of 52 strains of 13 species of Malassezia against 11 commonly used antifungals. MIC values determined by visual reading were in good agreement with MIC values determined by fluorescence reading. The lowest MICs were found for the azoles itraconazole, posaconazole and voriconazole with MIC90 values of 0.03-1.0 μg/ml, 0.06-0.5 μg/ml and 0.03-2.0 μg/ml, respectively. All Malassezia spp. were resistant to echinocandins and griseofulvin. Some Malassezia spp. also showed high MIC values for ketoconazole, which is the most widely recommended topical antifungal to treat Malassezia skin infections. In summary, our assay enables the fast and reliable susceptibility testing of Malassezia spp. against a large panel of different antifungals.
======================================================
14.) Pityriasis versicolor: an update on pharmacological treatment options.
======================================================
Expert Opin Pharmacother. 2014 Aug;15(12):1707-13. doi: 10.1517/14656566.2014.931373. Epub 2014 Jul 3.
Gupta AK1, Lyons DC.
Author information
1
University of Toronto, Department of Medicine , Toronto , Canada.
Abstract
INTRODUCTION:
Pityriasis versicolor (PV) is a superficial fungal infection caused by Malassezia species; a yeast that naturally colonizes on the skins surface. High efficacy rates are generally obtained with both topical and systemic treatments. However, recurrence rates following successful treatment remain high and there are no dosage guidelines available for administration of systemic antifungal agents that carry risks of adverse events.
AREAS COVERED:
This review focused on providing an overview of existing treatments for PV and an introduction to new treatments. A literature search was conducted using the search strategy, pityriasis versicolor OR tinea versicolor. Over the past decade, few new treatments have been introduced, but the efficacy and the dosing regimens of existing treatments have been systematically reviewed. The results of these reviews are discussed.
EXPERT OPINION:
Existing topical and systemic agents are both effective treatments against PV. Previous dosage recommendations for systemic agents have been modified based on recent evidence elucidated in systematic reviews. However, the absence of standardized collection and reporting practices in clinical trials precludes any conclusions to be drawn regarding the efficacy and safety of topical and systemic agents in comparison or in concert with each other.
===========================================================
15.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
===========================================================
Acta Derm Venereol Suppl (Stockh). 1979;(86):1-23.
Faergemann J.
Abstract
In patients with tinea versicolor, Pityrosporum orbiculare was cultured from tinea versicolor lesions in 100%, from normal-looking skin in 80%, and from apparently healed lesions in 69%. P. orbiculare was isolated from normal skin in 85% of patients with seborrheic dermatitis and in 90% of volunteers. The best substrate for isolation of P. orbiculare was a peptone-glucose-yeast extract medium containing glycerol monostearate and Tween 80, overlaid with olive oil. Germ tubes were produced when P. orbiculare was incubated in an atmosphere containing air with 7% CO2. Cultures of P. orbiculare and P. ovale did not show any fluorescence in Wood's light. The in vitro activity of miconazole, clotrimazole, econazole, sodium omadine, and sodium thiosulphate against P. orbiculare was found to correlate to the good clinical effect of these drugs in tinea versicolor. In addition several substances used as solvents or in vehicles had an inhibitory activity against P. orbiculare in vitro. Inoculation with P. orbiculare under plastic occlusion on the glabrous follicle-rich inside of the rabbit ear resulted in a tinea versicolor-like lesion after I week in 3 of 4 animals. One week after inoculation with P. orbiculare under plastic occlusion, experimental infections similar to those found clinically in tinea versicolor were seen in 10 of 12 patients with a history of tinea versicolor and in 3 of 6 normal volunteers. It was not possible to produce experimental infections without occlusion. Spontaneous healing usually occurred. In a retrospective study of 232 patients and prospective survey of 48 patients regarding susceptibility factors in tinea versicolor a higher (10.4%) than expected (3.8%) connection to seborrheic dermatitis was found.
===========================================================
16.) Tinea versicolor and Pityrosporum orbiculare: mycological investigations, experimental infections and epidemiological surveys.
===========================================================
Acta Derm Venereol Suppl (Stockh). 1979;(86):1-23.
Faergemann J.
Abstract
In patients with tinea versicolor, Pityrosporum orbiculare was cultured from tinea versicolor lesions in 100%, from normal-looking skin in 80%, and from apparently healed lesions in 69%. P. orbiculare was isolated from normal skin in 85% of patients with seborrheic dermatitis and in 90% of volunteers. The best substrate for isolation of P. orbiculare was a peptone-glucose-yeast extract medium containing glycerol monostearate and Tween 80, overlaid with olive oil. Germ tubes were produced when P. orbiculare was incubated in an atmosphere containing air with 7% CO2. Cultures of P. orbiculare and P. ovale did not show any fluorescence in Wood's light. The in vitro activity of miconazole, clotrimazole, econazole, sodium omadine, and sodium thiosulphate against P. orbiculare was found to correlate to the good clinical effect of these drugs in tinea versicolor. In addition several substances used as solvents or in vehicles had an inhibitory activity against P. orbiculare in vitro. Inoculation with P. orbiculare under plastic occlusion on the glabrous follicle-rich inside of the rabbit ear resulted in a tinea versicolor-like lesion after I week in 3 of 4 animals. One week after inoculation with P. orbiculare under plastic occlusion, experimental infections similar to those found clinically in tinea versicolor were seen in 10 of 12 patients with a history of tinea versicolor and in 3 of 6 normal volunteers. It was not possible to produce experimental infections without occlusion. Spontaneous healing usually occurred. In a retrospective study of 232 patients and prospective survey of 48 patients regarding susceptibility factors in tinea versicolor a higher (10.4%) than expected (3.8%) connection to seborrheic dermatitis was found.
===========================================================
17.) Mycological Considerations in the Topical Treatment of Superficial Fungal Infections.
===========================================================
J Drugs Dermatol. 2016 Feb;15(2 Suppl):s49-55.
Rosen T.
Abstract
Trichophyton rubrum remains the most common pathogenic dermatophyte in the United States, Europe, and industrialized Asia, although other species are predminant elsewhere. Candida albicans is the most common pathogenic yeast, with other species occasionally encountered. Just a few of the 14 described species of Malassezia cause pityriasis versicolor worldwide. FDA approval does not always accurately reflect the potential utility of any given topical antifungal agent. Azole, hydroxypyridone, and allylamine agents are beneficial in the management of dermatophytosis; however, the allylamines may lead to faster symptom resolution and a higher degree of sustained response. Although in actual clinical use the allylamines have all shown some activity against superficial cutaneous candidiasis and pityriasis versicolor, the azole agents remain drugs of choice. Ciclopirox is an excellent broad-spectrum antifungal agent. Optimal topical therapy for superficial fungal infections cannot yet be reliably based upon in-vitro laboratory determination of sensitivity. Inherent antibacterial and anti-inflammatory properties possessed by some antifungal agents may be exploited for clinical purposes. Candida species may be azole-insensitive due to efflux pumps or an altered target enzyme. So-called "antifungal resistance" of dermatophyets is actually due to poor patient adherence (either in dosing or treatment duration), or to reinfection.
===========================================================
18.) Single-dose fluconazole versus itraconazole in pityriasis versicolor.
===========================================================
Dermatology. 2004;208(1):55-9.
Partap R1, Kaur I, Chakrabarti A, Kumar B.
Author information
1
Department of Dermatology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Abstract
BACKGROUND:
The new antifungal triazoles itraconazole and fluconazole have revolutionized the treatment of pityriasis versicolor. Both drugs have shown promising results in different dose schedules.
OBJECTIVE:
To compare the efficacy and safety of single oral dose treatment with fluconazole versus itraconazole in patients with pityriasis versicolor.
METHODS:
A total of 40 patients with pityriasis versicolor were allocated randomly to group A and group B. A single dose of fluconazole (400 mg) or itraconazole (400 mg) was given orally to group A or group B patients, respectively. Patients were assessed mycologically by KOH and culture. Culture was done from lesional and perilesional skin to quantify growth and to observe the effect of these drugs and the persistence/reappearance of the fungus in relation to relapse at 2 and 8 weeks. Relapse was defined as reappearance or worsening of clinical signs and symptoms or positive KOH/culture after initial improvement.
RESULTS:
Thirteen (65%) patients in the fluconazole group and 4 (20%) patients in the itraconazole group became culture negative at the end of 8 weeks. Relapse was found to be higher in the itraconazole group compared to the fluconazole group (60 vs. 35%). A direct correlation was found between the relapse rate and positivity of perilesional skin for Malassezia furfur.
CONCLUSION:
In the same dosing, fluconazole was found to be more effective than itraconazole; however, both drugs were found to be safe.
===========================================================
19.) Itraconazole in tinea versicolor: a review.
===========================================================
J Am Acad Dermatol. 1990 Sep;23(3 Pt 2):551-4.
Delescluse J1.
Author information
1
Department of Dermatology, Clinic Cesar De Paepe, Brussels, Belgium.
Abstract
Itraconazole, a new orally active triazole antifungal, has been tested in patients with pityriasis versicolor. A number of studies have shown that itraconazole is effective for this mild fungal skin disease. The total dose required for effective treatment is 1000 mg, and it has been given as 200 mg for 5 days or 7 days. The organisms disappear slowly from the skin, even when dead, and the results should be assessed clinically and mycologically at around 3 to 4 weeks after treatment. Numerous studies have shown that itraconazole is superior to placebo and as effective as selenium sulfide, clotrimazole, and ciclopirox olamine. It is also better tolerated by patients than selenium sulfide.
===========================================================
20.) [Cutaneous Malassezia infections and Malassezia associated dermatoses: An update].
===========================================================
Hautarzt. 2015 Jun;66(6):465-84; quiz 485-6. doi: 10.1007/s00105-015-3631-z.
[Article in German]
Nenoff P1, Krüger C, Mayser P.
Author information
1
Labor für medizinische Mikrobiologie, Partnerschaft Prof. Dr. med. Pietro Nenoff & Dr. med. Constanze Krüger, Straße des Friedens 8, 04579, Mölbis, Deutschland, nenoff@mykologie-experten.de.
Abstract
The lipophilic yeast fungus Malassezia (M.) spp. is the only fungal genus or species which is part of the physiological human microbiome. Today, at least 14 different Malassezia species are known; most of them can only be identified using molecular biological techniques. As a facultative pathogenic microorganism, Malassezia represents the causative agent both of superficial cutaneous infections and of blood stream infections. Pityriasis versicolor is the probably most frequent infection caused by Malassezia. Less common, Malassezia folliculitis occurs. There is only an episodic report on Malassezia-induced onychomycosis. Seborrhoeic dermatitis represents a Malassezia-associated inflammatory dermatosis. In addition, Malassezia allergenes should be considered as the trigger of "Head-Neck"-type atopic dermatitis. Ketoconazole possesses the strongest in vitro activity against Malassezia, and represents the treatment of choice for topical therapy of pityriasis versicolor. Alternatives include other azole antifungals but also the allylamine terbinafine and the hydroxypyridone antifungal agent ciclopirox olamine. "Antiseborrhoeic" agents, e.g. zinc pyrithione, selenium disulfide, and salicylic acid, are also effective in pityriasis versicolor. The drug of choice for oral treatment of pityriasis versicolor is itraconazole; an effective alternative represents fluconazole. Seborrhoeic dermatitis is best treated with topical medication, including topical corticosteroids and antifungal agents like ketoconazole or sertaconazole. Calcineurin inhibitors, e.g. pimecrolimus and tacrolimus, are reliable in seborrhoeic dermatitis, however are used off-label.
===========================================================
21.) A double-blind comparative study of sodium sulfacetamide lotion 10% versus selenium sulfide lotion 2.5% in the treatment of pityriasis (tinea) versicolor.
============================================================
Cutis. 2004 Jun;73(6):425-9.
Hull CA1, Johnson SM.
Author information
1
Department of Dermatology, University of Arkansas for Medical Sciences, Little Rock, AR 72205, USA.
Abstract
Pityriasis (tinea) versicolor, which consists of hyperpigmented and hypopigmented scaly patches, is often difficult to treat. A double-blind comparative study between once-a-day sodium sulfacetamide lotion and selenium sulfide lotion was undertaken. Both treatments were safe and efficacious. Selenium sulfide was statistically more efficacious (76.2% vs 47.8%, P=.013).
===========================================================
22.) Selenium sulfide in tinea versicolor: blood and urine levels.
===========================================================
J Am Acad Dermatol. 1984 Aug;11(2 Pt 1):238-41.
Sánchez JL, Torres VM.
Abstract
The safety of topical selenium sulfide lotion in man has been demonstrated previously. Twenty male patients with a diagnosis of tinea versicolor were randomly assigned to two parallel groups who applied selenium sulfide lotion or the vehicle to the entire skin surface, excluding mucous membranes, for 10 minutes once daily for 7 consecutive days. Blood and urine selenium levels were determined before and after treatment and showed no significant differences between the active drug and vehicle groups on any study day. It would appear that no significant absorption of selenium took place as a result of this treatment regimen.
===========================================================
23.) New Antifungal Agents and New Formulations Against Dermatophytes.
===========================================================
Mycopathologia. 2017 Feb;182(1-2):127-141. doi: 10.1007/s11046-016-0045-0. Epub 2016 Aug 8.
Gupta AK1,2, Foley KA3, Versteeg SG3.
Author information
1
Department of Medicine, University of Toronto, Toronto, Canada. publications@mediproberesearch.com.
2
Mediprobe Research Inc., 645 Windermere Road, London, ON, Canada. publications@mediproberesearch.com.
3
Mediprobe Research Inc., 645 Windermere Road, London, ON, Canada.
Abstract
A variety of oral and topical antifungal agents are available for the treatment of superficial fungal infections caused by dermatophytes. This review builds on the antifungal therapy update published in this journal for the first special issue on Dermatophytosis (Gupta and Cooper 2008;166:353-67). Since 2008, there have not been additions to the oral antifungal armamentarium, with terbinafine, itraconazole, and fluconazole still in widespread use, albeit for generally more severe or recalcitrant infections. Griseofulvin is used in the treatment of tinea capitis. Oral ketoconazole has fallen out of favor in many jurisdictions due to risks of hepatotoxicity. Topical antifungals, applied once or twice daily, are the primary treatment for tinea pedis, tinea corporis/tinea cruris, and mild cases of tinea unguium. Newer topical antifungal agents introduced include the azoles, efinaconazole, luliconazole, and sertaconazole, and the oxaborole, tavaborole. Research is focused on developing formulations of existing topical antifungals that utilize novel delivery systems in order to enhance treatment efficacy and compliance.
===========================================================
24.) Tavaborole, Efinaconazole, and Luliconazole: Three New Antimycotic Agents for the Treatment of Dermatophytic Fungi.
===========================================================
J Pharm Pract. 2016 Aug 3. pii: 0897190016660487. [Epub ahead of print]
Saunders J1, Maki K1, Koski R2, Nybo SE3.
Author information
1
College of Pharmacy, Ferris State University, Big Rapids, MI, USA.
2
UP Health System Marquette, Marquette, MI, USA.
3
College of Pharmacy, Ferris State University, Big Rapids, MI, USA ericnybo@ferris.edu.
Abstract
Fungal diseases of the nail bed (onychomycosis) and epidermis are recurrent illnesses in the elderly and immunocompromised patients, which have few efficacious treatment options. Current treatment options for onychomycosis are limited to topical agents, laser treatment, and oral antifungals. Previous generations of topical agents were not efficacious, owing to poor penetration of the nail bed. Oral antifungal drugs, such as itraconazole, terbinafine, and fluconazole, not only give better response rates but also inhibit a host of CYP450 enzymes. Oral antifungals can exacerbate drug-drug interactions for patients taking other medications concurrently. Newer topical agents might recognize improved efficacy and provide therapeutic alternatives when the use of oral antifungal agents is contraindicated. Recently, the Food and Drug Administration (FDA) approved efinaconazole and tavaborole for the treatment of onychomycosis. Additionally, the FDA approved luliconazole for the treatment of tinea pedis, tinea cruris, and tinea corporis. This review examines the mechanism of action, spectrum of activity, pharmacokinetics, and clinical trials data and considers the place in therapy for these 3 new antimycotic agents.
===========================================================
25.) Therapeutic efficacy and safety of the new antimycotic sertaconazole in the treatment of Pityriasis versicolor.
===========================================================
Arzneimittelforschung. 1992 May;42(5A):764-7.
Nasarre J1, Umbert P, Herrero E, Roset P, Márquez M, Torres J, Ortiz JA.
Author information
1
Dermatology Department, Hospital Sagrado Corazón, Medical School, University of Barcelona, Spain.
Abstract
The activity of 7-chloro-3-[1-(2,4-dichlorophenyl)-2-(1H-imidazol-1-yl) ethoxy-methyl]benzo[b]thiophene (sertaconazole, FI-7045, CAS 99592-32,2) was studied in a randomized parallel double-blind clinical trial on 21 patients suffering from Pityriasis versicolor (confirmed by KOH microscopic examination and exploration with Wood's light). The patients were divided into two treatment groups: one with 11 patients receiving sertaconazole 1% cream and the other with 10 patients receiving sertaconazole 2% cream. The cream was applied twice a day during 4 weeks. The data were assessed clinically and microscopically (optical and fluorescence). All the patients were cured (100% cure), showing excellent efficacy. A check-up performed after the end of the treatment showed no relapses of infection. The drug safety was optimum, since no local or general undesirable effects were recorded, nor were there any changes in the analytical parameters studied in the 21 patients. Because of its high antifungal activity and excellent safety, sertaconazole represents an important advance in the topical therapy of this disease.
===========================================================
25.) Whole genome sequencing analysis of the cutaneous pathogenic yeast Malassezia restricta and identification of the major lipase expressed on the scalp of patients with dandruff.
===========================================================
Mycoses. 2017 Mar;60(3):188-197. doi: 10.1111/myc.12586. Epub 2016 Nov 24.
Park M1, Cho YJ2, Lee YW3,4, Jung WH1.
Author information
1
Department of Systems Biotechnology, Chung-Ang University, Anseong, Korea.
2
ChunLab, Inc., Seoul National University, Seoul, Korea.
3
Department of Dermatology, School of Medicine, Konkuk University, Seoul, Korea.
4
Research Institute of Medical Science, Konkuk University, Seoul, Korea.
Abstract
Malassezia species are opportunistic pathogenic fungi that are frequently associated with seborrhoeic dermatitis, including dandruff. Most Malassezia species are lipid dependent, a property that is compensated by breaking down host sebum into fatty acids by lipases. In this study, we aimed to sequence and analyse the whole genome of Malassezia restricta KCTC 27527, a clinical isolate from a Korean patient with severe dandruff, to search for lipase orthologues and identify the lipase that is the most frequently expressed on the scalp of patients with dandruff. The genome of M. restricta KCTC 27527 was sequenced using the Illumina MiSeq and PacBio platforms. Lipase orthologues were identified by comparison with known lipase genes in the genomes of Malassezia globosa and Malassezia sympodialis. The expression of the identified lipase genes was directly evaluated in swab samples from the scalps of 56 patients with dandruff. We found that, among the identified lipase-encoding genes, the gene encoding lipase homolog MRES_03670, named LIP5 in this study, was the most frequently expressed lipase in the swab samples. Our study provides an overview of the genome of a clinical isolate of M. restricta and fundamental information for elucidating the role of lipases during fungus-host interaction.
=========================================================================
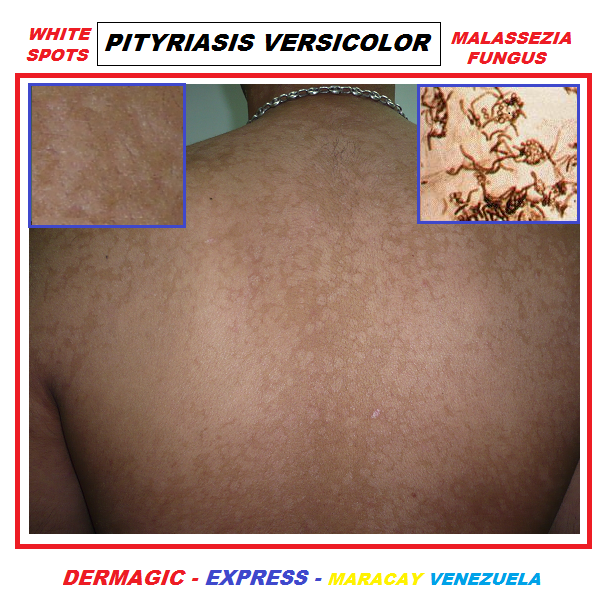






No hay comentarios:
Publicar un comentario
Tu comentario será objeto de revisión y luego aprobado.
Your comment will be revised and then approved.